J Clin Oncol:T-DM1+帕妥珠单抗 vs 紫杉类+曲妥珠单抗+帕妥珠单抗治疗高危HER2+早期乳腺癌患者的疗效和安全性:III期临床研究KAITLIN
2021-12-12 yd2015 MedSci原创
研究表明,T-DM1 +帕妥珠单抗(AC-KP)并不比紫杉烷+曲妥珠单抗+帕妥珠单抗(AC-THP) 改善患者IDFS。AC-THP仍是标准治疗方案。
抗HER2治疗是HER2阳性乳腺癌患者的基础治疗手段。近期,Journal of Clinical Oncology杂志上发表了III期临床研究KAITLIN (NCT01966471)的研究结果,其在高危HER2+早期乳腺癌(EBC)患者中,比较T-DM1+帕妥珠单抗和紫杉类+曲妥珠单抗+帕妥珠单抗治疗的疗效和安全性。

KAITLIN (NCT01966471)纳入HER2阳性EBC(淋巴结阳性或阴性,激素受体阴性,肿瘤>2cm)。患者被1:1随机分为两组:先进行蒽环类化疗(3 - 4个周期),然后分为T-DM1 +帕妥珠单抗(AC-KP)或紫杉烷(3 - 4个周期)+曲妥珠单抗+帕妥珠单抗(AC-THP) 18个周期。允许辅助放疗/内分泌治疗。主要终点是ITT淋巴结阳性和总体人群中的无浸润生存期(IDFS)。
2014年1月至2015年6月,共纳入1846例患者(AC-THP组918例; AC-KP 928例)。其中,有1658人(89.8%)是淋巴结阳性(AC-THP 826例; AC-KP 832例)。AC-THP组中位随访时间为57.1个月(52.1-60.1个月),AC-KP组中位随访时间为57.0个月(52.1- 59.8个月)。
淋巴结阳性患者中,与AC-THP相比,AC-KP治疗并没有降低淋巴结阳性亚组患者IDFS风险(HR, 0.97;95% CI, 0.71 ~ 1.32;P=0.83)。AC-THP的3年IDFS率为94.1% (95% CI, 92.5 ~ 95.7), AC-KP的3年IDFS率为92.8% (95% CI, 91.0 ~ 94.5)。同样,总体人群中,与AC-THP相比,AC-KP也没有降低IDFS事件的风险(HR, 0.98;95% CI, 0.72 ~ 1.32)。AC-THP的3年IDFS率为94.2% (95% CI, 92.7 ~ 95.8), AC-KP的3年IDFS率为93.1% (95% CI, 91.4 ~ 94.7)。

淋巴结阳性和总体人群两治疗组的IDFS
在预先指定的探索性亚组分析中,除保乳手术的IDFS有差异外,不同亚组间的IDFS一致相似。保乳术治疗患者中,AC-THP和AC-KP组的3年IDFS率分别为95.6%和91.4%(HR=1.73,95% CI, 1.03-2.90)。OS数据不成熟,接受AC-THP和AC-KP治疗患者的OS事件发生率分别为3.6%和4.7%。
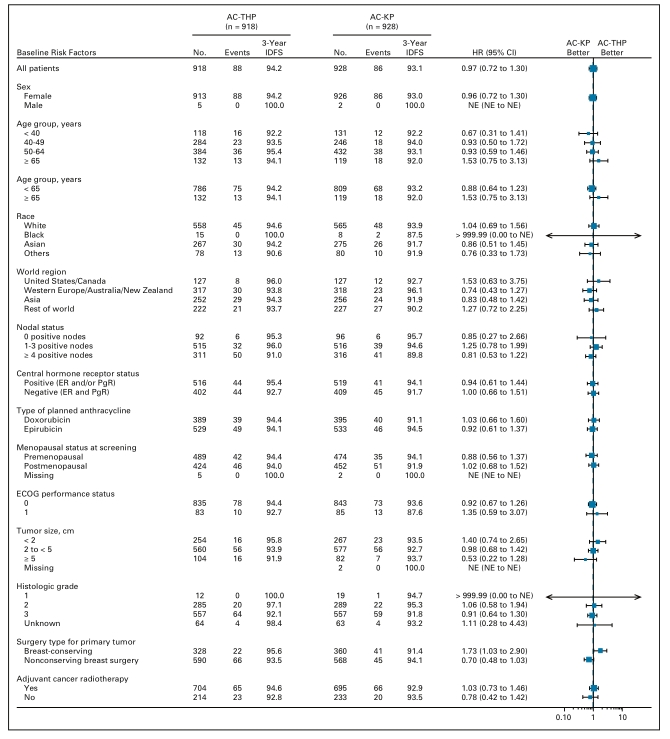
亚组分析的IDFS
AC-THP和AC-KP组≥3级AEs相似。导致曲妥珠单抗或T-DM1停用的AEs发生在接受AC-THP和AC-KP的患者中分别为4.0%和26.8%。导致紫杉烷停药的AEs发生在AC-THP患者中6.7%。
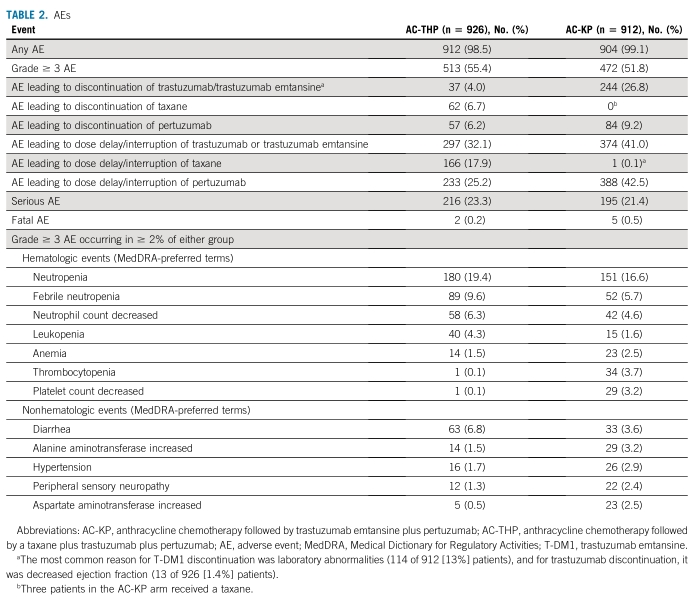
AEs
综上,研究表明,T-DM1 +帕妥珠单抗(AC-KP)并不比紫杉烷+曲妥珠单抗+帕妥珠单抗(AC-THP) 改善患者IDFS。AC-THP仍是标准治疗方案。
原始出处:
Krop IE, Im SA, Barrios C, Bonnefoi H, Gralow J, Toi M, Ellis PA, Gianni L, Swain SM, Im YH, De Laurentiis M, Nowecki Z, Huang CS, Fehrenbacher L, Ito Y, Shah J, Boulet T, Liu H, Macharia H, Trask P, Song C, Winer EP, Harbeck N. Trastuzumab Emtansine Plus Pertuzumab Versus Taxane Plus Trastuzumab Plus Pertuzumab After Anthracycline for High-Risk Human Epidermal Growth Factor Receptor 2-Positive Early Breast Cancer: The Phase III KAITLIN Study. J Clin Oncol. 2021 Dec 10:JCO2100896. doi: 10.1200/JCO.21.00896. Epub ahead of print. PMID: 34890214.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#AIT#
41
#曲妥珠#
50
#II期临床研究#
38
#Oncol#
28
#I期临床#
27
#III期临床研究#
32
#疗效和安全性#
20
#III#
27
学到了
39
#II期临床#
26