Sci Adv:牙周炎细菌导致阿尔茨海默病实锤!科学家发现导致牙周炎的细菌能轻易侵入大脑,分泌有害蛋白诱发AD
2019-01-27 奇点糕 奇点网
近日,加州大学旧金山分校的Stephen Dominy博士领导的团队证又发现,引起牙周炎的细菌——牙龈卟啉菌,同样会导致AD。这些研究都指向同一个方向——病原体感染,可能才是导致AD的真正元凶!
2018年以来,科学界最大的亮点可能就是阿尔茨海默病(AD)的感染致病理论了。
去年6月,我们曾报道科学家发现疱疹病毒可能才是AD的致病因素;前不久,我们又报道了会引起口腔溃疡的白色念珠菌可以引起疑似AD的病征。
近日,加州大学旧金山分校的Stephen Dominy博士领导的团队证又发现,引起牙周炎的细菌——牙龈卟啉菌,同样会导致AD。这些研究都指向同一个方向——病原体感染,可能才是导致AD的真正元凶!
在这个研究中,Stephen团队先是在AD患者的大脑中检测到了牙龈卟啉菌的存在,又通过小鼠实验证实牙龈卟啉菌进入大脑后释放的一种分泌蛋白才是导致AD的关键。随后,他们在人体中还发现抑制该蛋白能够起到治疗AD的作用。此外,该团队还证实,β-淀粉样蛋白具有抗细菌感染的作用。
这个研究可能指导我们透过表象(tau蛋白和β-淀粉样蛋白沉积等),找到AD真正的病因,进而找到治疗AD的办法。相关论文发表在著名学术期刊Science Advance上。

Stephen Dominy博士
这些年来,学界对AD研究的重点一直是tau蛋白和β-淀粉样蛋白沉积等,但是针对这些蛋白的药物的临床试验却几度碰壁。这也让相关领域一直被悲观的情绪所笼罩。
不过,也一直有科学家在迷茫旷野中寻找新的出路。
除了tau蛋白和β-淀粉样蛋白沉积这些典型的特征外,AD病人还会表现出神经炎症,这和病原体感染的症状很像。所以,也有人怀疑感染才是AD的病因,但却找不到切实可靠的证据。
Stephen Dominy博士在上世纪90年代时,曾在加州大学旧金山分校治疗HIV携带者。当时,他发现一些因HIV导致认知障碍的患者,在接受抗病毒药物治疗后,认知能力恢复了。这让他对AD感染理论产生了强烈的兴趣。
早有证据表明,牙齿脱落、牙周疾病和AD有很深的联系。而牙龈卟啉菌也被认为是β-淀粉样蛋白沉积、痴呆、AD的高危风险因素。一项前瞻性观察研究显示,相比对照组,有慢性牙周炎的患者在6个月内认知能力有明显下降。
并且,科学家还发现牙龈卟啉菌可以在冠状动脉、胎盘及肝脏中定植。而牙龈卟啉菌在人体内横行无忌的原因之一,就是它能分泌一种牙龈蛋白酶。这个牙龈蛋白酶具有帮助细菌定植,压制宿主免疫系统,以及破坏组织等多种作用,并对很多细胞具有毒性。
牙龈卟啉菌
鉴于牙龈卟啉菌与AD有如此紧密的联系,Stephen博士和合作者开办了一家公司,研究对AD的治疗。他将目标锁定在牙龈卟啉菌身上,并在AD死者大脑中寻找牙龈卟啉菌。
研究人员先是检测了AD死者的大脑样本,发现所有的样本中都有牙龈卟啉菌。随后,他们又检测了具有轻度至中度认知障碍的疑似AD患者的脑脊液,同样也发现大部分患者的大脑中都有牙龈卟啉菌感染。这说明牙龈卟啉菌确实能进入大脑,并在大脑中定植。
前面我们提到过,牙龈蛋白酶是牙龈卟啉菌的毒性因子。科学家猜测,如果牙龈卟啉菌是AD的病因的话,那么其分泌牙龈蛋白酶可能会损伤神经。
实验结果证明确实如此。研究人员一共检测了50份AD死者的大脑样本,发现在超过90%的样本中都有牙龈蛋白酶的存在。这个蛋白遍及神经元、星形胶质细胞、受损的海马体以及大脑皮层,并且还发现其与tau蛋白和β-淀粉样蛋白沉积的位置重叠。
牙龈蛋白酶与tau蛋白和β-淀粉样蛋白沉积
随后,研究者在体外证明牙龈蛋白酶具有将tau蛋白切成碎片的功能。这说明,AD患者大脑中出现的tau蛋白缠结很可能就是牙龈蛋白酶引起的!牙龈卟啉菌引起AD的嫌疑极大。
那牙龈卟啉菌到底会不会引起AD呢?
研究人员通过动物实验进行了验证。他们让小鼠口腔感染牙龈卟啉菌,发现6周后,所有小鼠的大脑中都感染了牙龈卟啉菌,并且引发了β-淀粉样蛋白沉积。有意思的是,他们发现这些β-淀粉样蛋白具有抑制牙龈卟啉菌的作用,印证了之前β-淀粉样蛋白是抗菌斗士的研究。
前面提到过,牙龈蛋白酶可能是造成神经损伤的关键因素,若牙龈卟啉菌不能表达这个蛋白会怎样呢?研究人员将牙龈卟啉菌的牙龈蛋白酶编码基因敲除,然后用突变菌感染小鼠口腔,发现小鼠大脑内的病原菌明显降低,而β-淀粉样蛋白沉积也大幅减少。这说明牙龈蛋白酶对于牙龈卟啉菌引起AD是至关重要的。
而这还说明一个问题,那就是可以通过抑制牙龈蛋白酶来治疗AD!(广谱抗生素无法根除牙龈卟啉菌,且可能导致抗性)
Stephen团队找到了一种专门抑制牙龈蛋白酶的小分子抑制剂。将这个抑制剂给被感染的小鼠口服后,确实能起到保护小鼠大脑神经元,抑制细菌生长以及降低β-淀粉样蛋白沉积的作用。
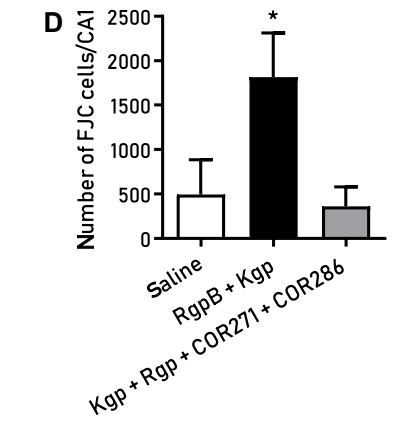
抑制牙龈蛋白酶可以保护海马体神经元
这是继疱疹病毒后,又一种病原体被明确证实会引发AD。同时,研究者们又一次验证了β-淀粉样蛋白的抗感染功能。越来越多地证据表明,AD可能是病原体感染引发的,而之前人们所关注的蛋白沉积可能仅仅是感染的结果。这或许能指导我们破除迷雾,找到AD的源头,彻底解决这个威胁着数千万人健康的疾病。
牙龈卟啉菌可能不是导致AD的唯一原因,但从研究者们提供的数据来看,可能也占据了相当的比例。因而,这个研究对于治疗AD有重要意义。
研究中所用到的小分子抑制剂COR388,在初步的临床研究中,有9名AD患者的认知得到改善。研究者表示,他们对这个结果感到鼓舞,后面将会组织临床Ⅱ/Ⅲ期试验。让我们期待Stephen博士的好消息。
所以,出于降低AD风险的考虑,大家也要勤刷牙、洗牙,保持口腔健康哦~
原始出处:Stephen S. Dominy, Casey Lynch1, Florian Ermini, et al. Porphyromonas gingivalis in Alzheimer’s disease brains: Evidence for disease causation and treatment with small-molecule inhibitors. Sci Adv, 23 Jan 2019
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#分泌#
27
#阿尔茨海#
27
#科学家发现#
26
#阿尔茨#
0
#牙周#
33
#阿尔茨海默#
24