Blood:根据治疗间期PET/CT扫描结果,予以早期霍奇金淋巴瘤患者风险适应性的治疗
2018-08-03 MedSci MedSci原创
中心点:间期PET扫描阴性的小肿块的I/II期霍奇金淋巴瘤患者,进行4个疗程的ABVD治疗,无放疗,3年无进展存活率可达91%。摘要:新确诊的小肿块的I/II期霍奇金淋巴瘤(HL)患者,进行1-3个疗程的阿霉素、博来霉素、长春花碱和达卡巴嗪(ABVD)治疗后,行PET/CT检查阴性,提示复发风险低。David J. Straus等人开展一2期临床试验,探1日,究早期患者人群是否可以在PET/CT阴
间期PET扫描阴性的小肿块的I/II期霍奇金淋巴瘤患者,进行4个疗程的ABVD治疗,无放疗,3年无进展存活率可达91%。
摘要:
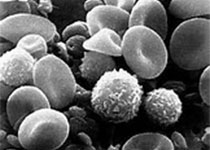
新确诊的小肿块的I/II期霍奇金淋巴瘤(HL)患者,进行1-3个疗程的阿霉素、博来霉素、长春花碱和达卡巴嗪(ABVD)治疗后,行PET/CT检查阴性,提示复发风险低。David J. Straus等人开展一2期临床试验,探1日,究早期患者人群是否可以在PET/CT阴性的基础上,进行短疗程的ABVD治疗,而不进行放疗(RT),从而减少治疗的副作用。
2010年5月15日-2013年2月21日,共招募了164位未进行过治疗的小肿块的I/II期HL患者,其中149位被纳入最终的分析。患者进行2个疗程的ABVD治疗后,予以PET扫描。Deauville评分1-3分为阴性。PET扫描阴性的患者继续接受2个疗程的ABVD,而PET扫描阳性的患者接受2个疗程的剂量增强的博来霉素、依托泊苷、阿霉素、环磷酰胺、长春新碱、甲苄肼和强的松(升级版BEACOPP)+3060cGy局部放疗(IF RT)。
主要结点是明确PET-阴性组患者的3年无进展存活率(PFS)。135位患者为PET扫描阴性(91%),14位为PET扫描阳性(9%)。中位随访3.8年,PET-阴性组的3年无进展存活率为91%,而PET-阳性组的仅66%(p=0.011),风险比3.84[1.50,9.84]。一位患者自杀死亡。对于大部分早期小肿块的、治疗间期PET扫描阴性的HL患者,4个疗程的ABVD治疗可获得持久的缓解。
原始出处:
David J. Straus, et al. CALGB 50604: risk-adapted treatment of nonbulky early-stage Hodgkin lymphoma based on interim PET. Blood 2018 :blood-2018-01-827246; doi: https://doi.org/10.1182/blood-2018-01-827246
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#PE#
27
#PET/CT#
43
#PET#
26
#CT扫描#
33
#适应性#
37
学习谢谢分享
54