JACC很大样本肥厚心肌病注册:36%有肌节蛋白基因突变
2019-11-25 xujing 中国循环杂志
JACC发表全球全球最大规模的肥厚性心肌病注册研究数据提示,36%患者存在心肌肌节蛋白基因突变,心肌肌节蛋白基因突变阳性和突变阴性的病变特点不同。研究者发现,肌节突变阳性患者更有可能出现室间隔反曲形态,纤维化较多,但静息性梗阻较少。肌节突变阴性者更易出现基底间隔肥大,但纤维化较少。研究者首次将高科技成像、基因分析和生物标志物数据与传统临床信息相结合,以便于对肥厚型心肌病进行最复杂的分析。18%的患
JACC发表全球全球最大规模的肥厚性心肌病注册研究数据提示,36%患者存在心肌肌节蛋白基因突变,心肌肌节蛋白基因突变阳性和突变阴性的病变特点不同。
研究者发现,肌节突变阳性患者更有可能出现室间隔反曲形态,纤维化较多,但静息性梗阻较少。
肌节突变阴性者更易出现基底间隔肥大,但纤维化较少。
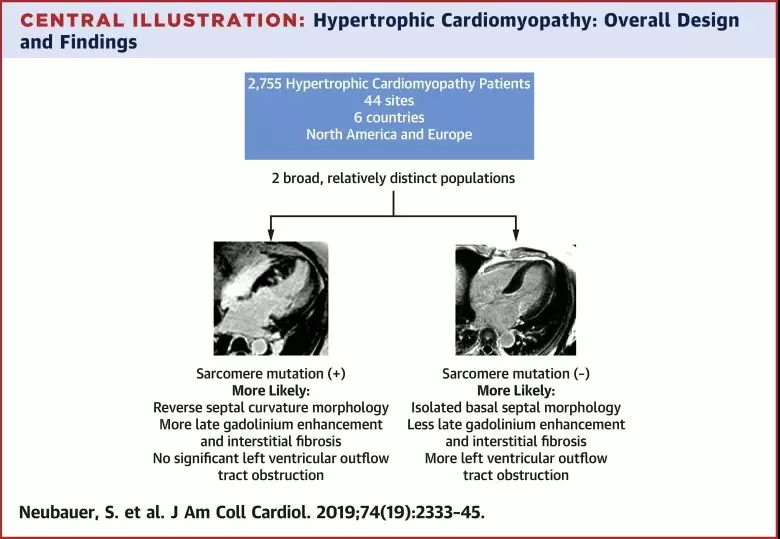
研究者首次将高科技成像、基因分析和生物标志物数据与传统临床信息相结合,以便于对肥厚型心肌病进行最复杂的分析。
18%的患者静息左室流出道(LVOT)梯度≥30 mmHg。36%的人有心肌肌节蛋白基因突变,50%有心肌纤维化。
该组患者具有低风险肥厚型心肌病的特点,93%没有或只有轻微的功能受限。
研究纳入2755名肥厚型心肌病患者,平均年龄(49±11)岁,71%为男性,平均ESC危险评分为(2.48±0.56)分。
研究还在进行中,研究者称,进一步的随访将有助于更好地了解亚组特点,并开发一个包含所有疾病信息的风险预测模型。
来源:Stefan Neubauer, et al. Distinct Subgroups in Hypertrophic Cardiomyopathy in the NHLBI HCM Registry. Distinct Subgroups in Hypertrophic Cardiomyopathy in the NHLBI HCM Registry. J Am Coll Cardiol, 2019, 74: 2333.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#JACC#
18
#样本#
19
#ACC#
22
#注册#
35
#肌病#
24