JAHA:纤维性肌发育不良患者性别与颈动脉夹层之间的相关性
2021-05-17 MedSci原创 MedSci原创
在FMD患者中,除其他既往已知的危险因素外,男性和多部位受累也与CeAD有关。
颈动脉夹层(CeAD)是纤维肌发育不良(FMD)患者较为常见的临床表现。但是,CeAD的危险因素尚未明确。

近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,研究人员在肾脏和颈动脉发育不良评估(ARCADIA)登记中心调查了与CeAD相关的因素。

ARCADIA登记中心纳入了年龄≥18岁,诊断为肾、颈或颅内动脉FMD的女性或男性,这些参与者是从法国和比利时的16所大学教学医院中前瞻性招募的。根据诊断标准,在影像学检查中确定了急性或既往CeAD的诊断。研究人员通过Logisitic回归分析对潜在决定因素与CeAD之间的关联进行了评估。
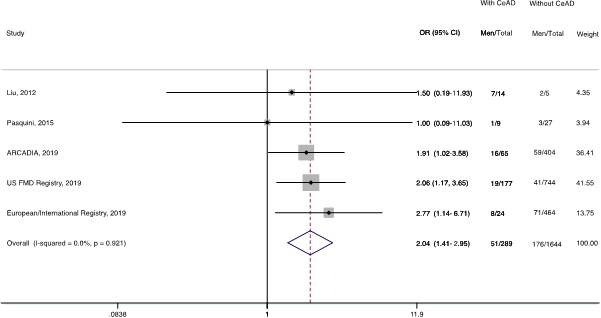
在469名FMD患者(75名男性)中,65名(13.9%)患者伴有CeAD。与没有CeAD的患者相比,CeAD患者更年轻,更有可能为男性,以及伴有偏头痛史,且无高血压病史。在多变量分析中,男性(比值比[OR]为2.66;95%CI为1.34-5.25)、偏头痛病史(OR为1.90;95%CI为1.06-3.39)、年龄≥50岁(OR为0.41;95%CI为0.23-0.73)、高血压病史(OR为0.35;95%CI为0.20-0.64)、3处以上血管床受累(OR为2.49;95%CI为1.15-5.40)与CeAD之间显著相关。为了验证CeAD与性别之间的关联,研究人员进行了系统评价,从2篇已发表的研究中收集了有关性别的其他数据,并从美国纤维肌发育不良登记中心和欧洲/国际FMD登记中心收集了未发表的数据。在汇总分析(289例CeAD病例,1933例患者)中,男性与CeAD之间显著相关(OR为2.04;95%CI为1.41-2.95;I2=0%)。
由此可见,在FMD患者中,除其他既往已知的危险因素外,男性和多部位受累也与CeAD有关。
原始出处:
Charlotte Arnaud.et al.Male Sex Is Associated With Cervical Artery Dissection in Patients With Fibromuscular Dysplasia.J AM HEART ASSOC.2021.https://www.ahajournals.org/doi/10.1161/JAHA.120.018311
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#颈动脉#
37
#相关性#
33
#颈动脉夹层#
48
#AHA#
38
#发育#
42
#动脉夹层#
36
#发育不良#
40
学习学习
62