Neurology:神经节后超声检测的形态功能对比,有助于早期鉴别多系统萎缩(MSA-P)和帕金森病(PD)!
2022-02-11 Naomi MedSci原创
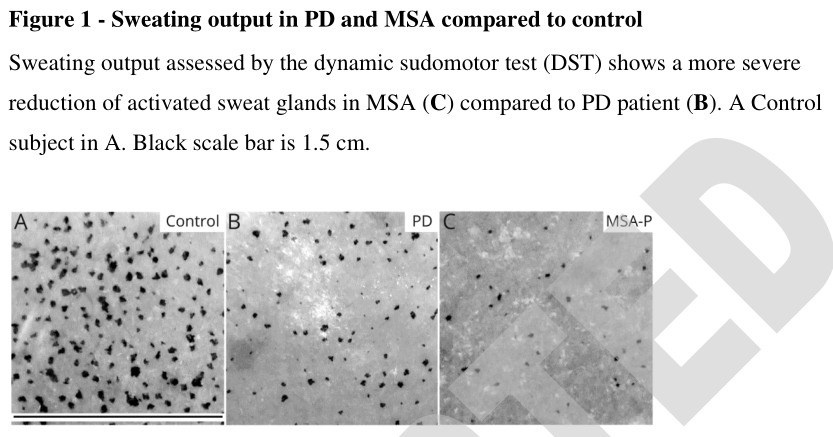
近日,有研究人员定量评估了动态汗液试验和皮肤自主神经,这一方法提供了一个敏感的形态功能方法以评估神经节后泌汗神经通路的组成部分:相较于PD,上述部分在疾病过程早期更多参与MSA-P。
”帕金森综合症“定义了一些临床症状,主要是伴随强直、震颤和运动迟缓等运动症状。这其中包含原发性帕金森病(PD),以及其他不同发病机制、预后和药物治疗反应的更多罕见综合征,如多系统萎缩症(MSA)。
帕金森综合症影响了65岁以上约2% 的人。缺乏改善疾病的治疗会导致严重的残疾,从而给全世界的卫生系统带来沉重的负担。在疾病过程中,症状和体征的出现和程度,以及随着时间的推移,更具体的神经影像特征的发展,可以分辨临床情况,并有助于达到既定的诊断标准以达到诊断。因此,即使对于运动障碍方面的专家,早期鉴别诊断仍是一项具有挑战性的任务。由于这些原因,能够帮助临床医生识别不同形式的帕金森综合征的早期生物标志物,是高度需要的。自主神经紊乱通常是帕金森综合征患者的主要症状,可以追溯到运动症状完全发展之前的许多年。泌汗神经障碍已被认为是一个关键特征,包括 MSA的节前和节后功能障碍,其严重程度与MSA小脑型相比更甚。然而,这些研究仅包括对疾病晚期患者的回顾性研究或前瞻性研究,而缺乏对疾病早期收缩功能障碍的前瞻性评价研究。
近日,有研究人员评估了早期(运动发病2年内)MSA-P和PD患者的前瞻性形态学和功能性自主神经辅助器的受累情况,以确定可能的生物标志物,以确定可能有助于早期鉴别这两种疾病的生物标志物。
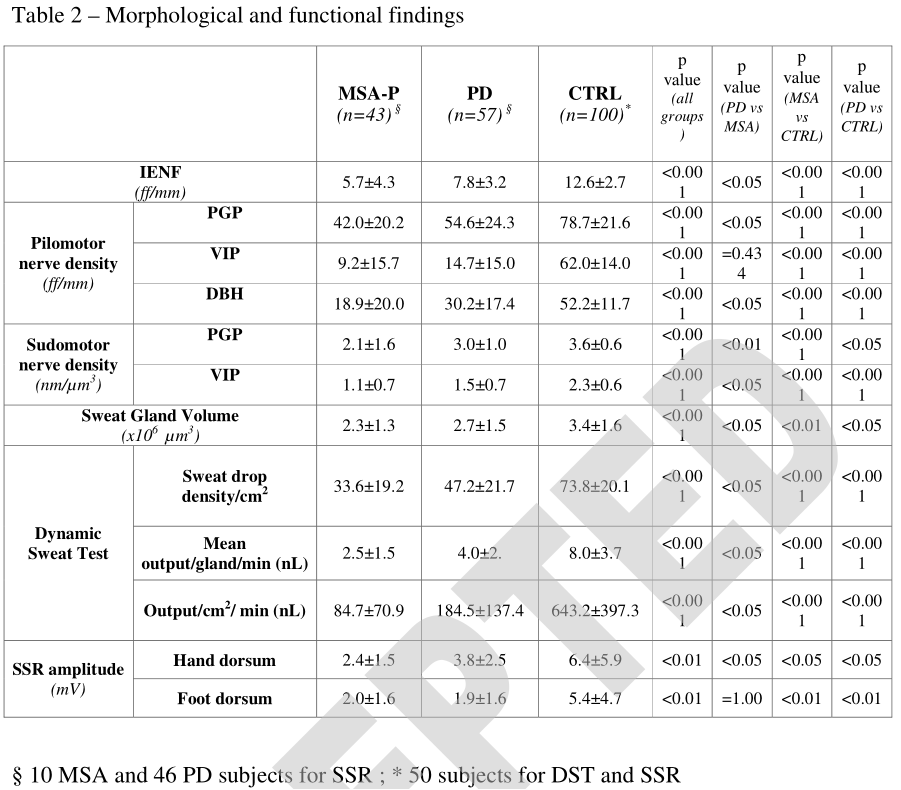
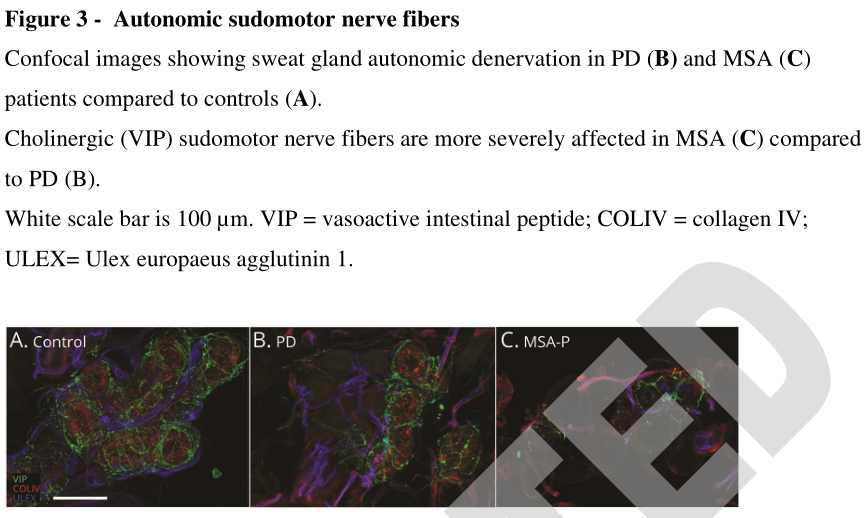
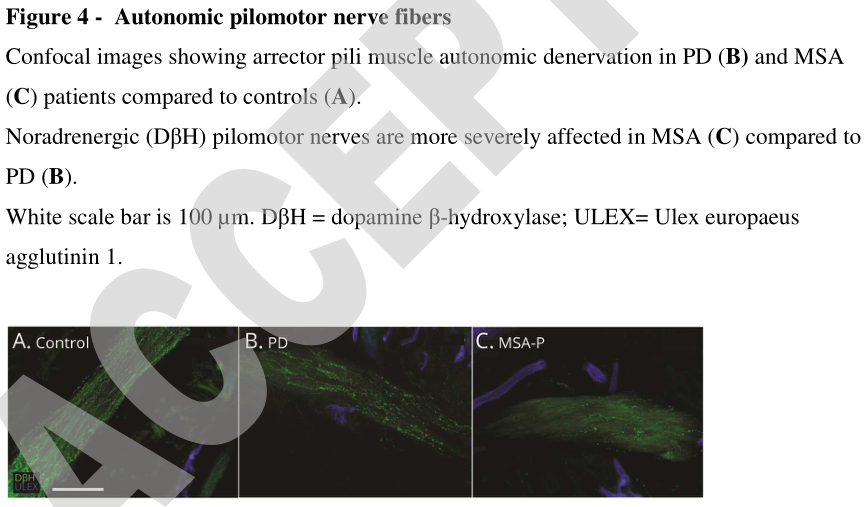
研究包括100例自运动症状发作2年内出现帕金森综合征的患者。招募时,采用问卷调查法评估患者的非运动、自主神经和小纤维症状,采用动态汗液试验和远端穿刺皮肤活检法评估患者的神经节后超音速功能。皮肤样本经处理后,以去甲肾上腺素能及胆碱能抗体作为间接免疫荧光。应用专用软件在共聚焦图像上测量表皮内、支座和毛运动神经纤维的密度。在招募后12个月进行随访以确认诊断。
- 57例 pd 患者(m/f = 36/21,年龄63.5 ± 9.4岁)和43例 MSA-P患者(m/f = 27/16,年龄62.3 ± 9.0岁)被纳入研究。
- 临床量表和问卷显示MSA-P患者的临床症状较PD患者严重。
- 出汗量和与对照组相比,两组的表皮内、毛运动神经和超毛运动神经密度都较低,但MSA-P患者的损害更大。
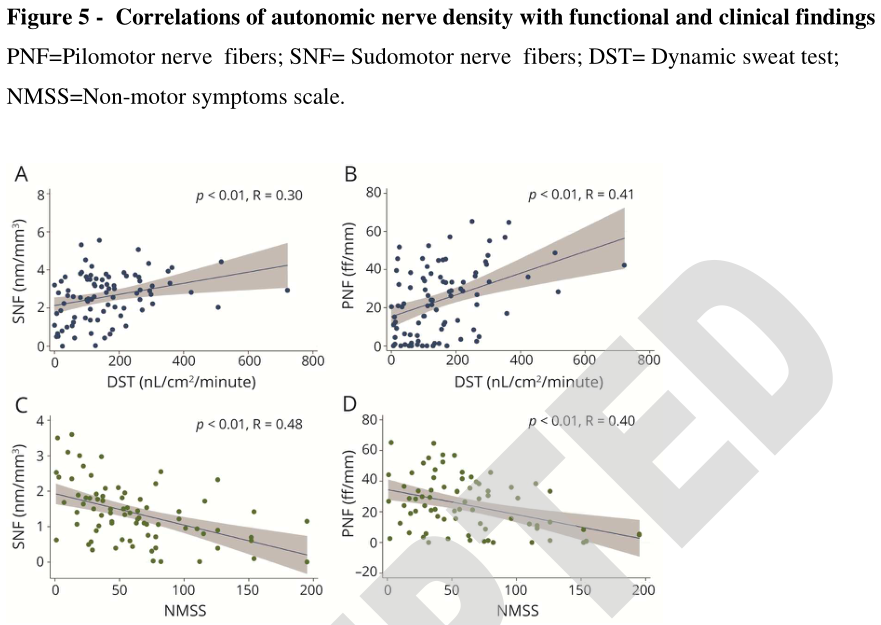
- 毛运动神经和超长运动神经密度与出汗功能和非运动性临床症状相关。
- 定义了汗液产生量乘以汗液纤维密度的算术乘积,有效地分离了两个种群,接收机工作特性曲线下面积为0.83。
动态汗液试验和皮肤自主神经的定量提供了一个敏感的形态功能方法来评估神经节后泌汗神经通路的组成部分,揭示了一个更严重的参与MSA-P比PD在疾病过程早期。这种方法可以用来早期区分这两种情况。
证据分类: 这项研究提供了 ii 类证据,神经节后形态功能评估准确地区分PD与MSA-P患者。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言

















#Neurol#
32
#萎缩#
27
坚持学习
49
学习#期刊论坛#
93
学习
54
#多系统萎缩#
30