Nat Med:肺癌早期诊断迎来新突破!有望在发病前就进行诊治
2019-01-22 佚名 学术经纬
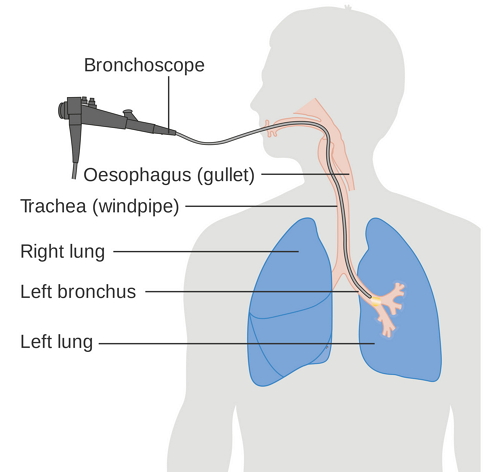
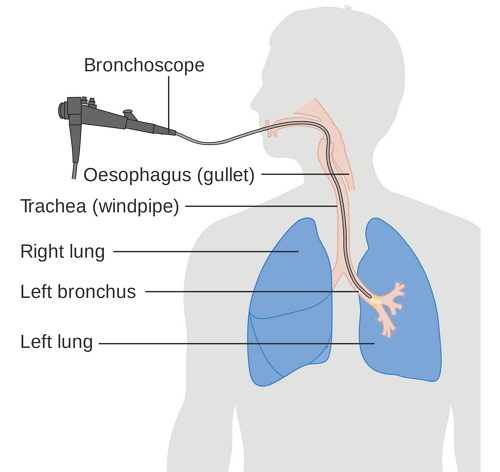
肺癌是全世界范围内,癌症致死的最主要原因之一。这一疾病之所以难治,很大一部分原因在于,患者在确诊时,病情已经进入了晚期。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#新突破#
31
#Nat#
33
#早期诊断#
35
#Med#
38
学习了,谢谢作者分享!
76
谢谢分享,学习了
1
离中国推广还有距离啊
69
厉害 这个作用超级大 不过在人口基数大的中国 这个意思推广还是艰巨
57