J Thromb Haemost:非瓣膜性房颤患者:利伐沙班vs阿哌沙班
2017-11-01 王淳 环球医学
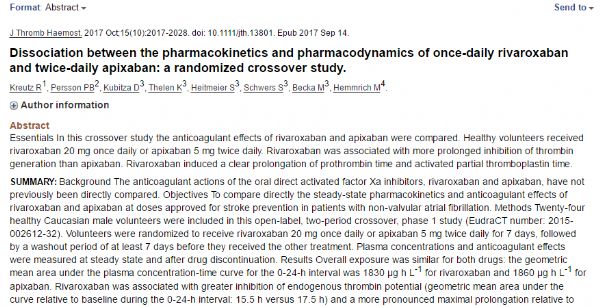
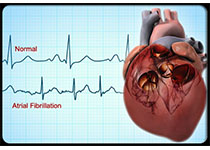
2017年10月,发表在《J Thromb Haemost》上的一项开放标签、2阶段随机交叉研究,对利伐沙班每日1次20 mg和阿哌沙班每日2次5 mg的药效学和药动学进行比较。研究结果证实:利伐沙班每日1次20 mg抑制凝血酶活性更强且持续时间更长。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#非瓣膜性房颤患者#
43
#HAE#
36
#瓣膜性#
38
#非瓣膜性#
39
#非瓣膜性房颤#
45
#瓣膜#
36
#房颤患者#
30