AJRCCM:DP1缺失通过mTORC1信号加重肺动脉高压的血管重构
2021-11-02 刘少飞 MedSci原创
肺动脉高压(PAH)是一种破坏性疾病,其特征是肺血管收缩,重塑及血栓形成。D 类前列腺素受体亚型 1(DP1) 受体的消融加剧了缺氧诱导的 PAH,并通过激活 mTORC1信号增强了小鼠的肺动脉重塑。

肺动脉高压 (PAH) 是一种进行性和致命的肺血管疾病,其特征是严重的远端肺动脉 (PA) 重构和肺血管阻力增加,最终导致右侧心力衰竭。 内皮功能障碍、平滑肌细胞增生和肥大、细胞外基质沉积和血管周围炎症浸润有助于 PAH 中的 PA 重塑。 目前可用的疗法如内皮素受体拮抗剂、磷酸二酯酶抑制剂和前列环素类似物主要针对肺血管收缩和改善 PAH 症状,但死亡率仍然不令人满意。 确定参与肺血管重塑的新途径可以揭示新的治疗靶点,从而改善临床结果。
花生四烯酸代谢物在维持肺血管稳态中起关键作用。环氧合酶 (COX) 催化花生四烯酸转化为前列腺素 (PG),包括 PGE2、PGD2、PGF2α 和 PGI2(前列环素)和血栓素,所有这些都通过激活同源 G 蛋白偶联来发挥其生理和病理生理功能受体(即 PGE2 受体、PGD2 受体 [D 前列腺素受体亚型 1 和 2;DP1 和 DP2]、PGF2α 受体、PGI2 受体 和血栓素受体)。
作为一种吸入药物,曲前列环素在相对较低的剂量下对肺血管阻力产生更持久的作用,耐受性比伊洛前列素更高,尽管半衰期更长,曲前列素对血管扩张剂 DP1 和 EP2 受体的亲和力比伊洛前列素高得多。一方面,DP1 在人肺动脉和静脉中均有表达,其激活会导致人肺血管松弛;另一方面,EP2 在体外抑制内皮素 1 刺激的人肺动脉平滑肌细胞 (hPASMC) 的增殖。因此,DP1 拮抗剂抑制曲前列环素诱导的人 PA 的松弛,表明它们可以介导曲前列环素对 PAH 患者的治疗作用。然而,DP1和EP2受体是否参与PAH的发病机制仍有待确定。
研究目的:研究DP1在PAH进展中的作用及其潜在机制。
研究方法:在患有 PAH 的患者和动物的肺动脉中检查 DP1 水平。多种遗传和药理学方法被用于研究多环芳烃中 DP1 介导的信号传导。
研究结果:
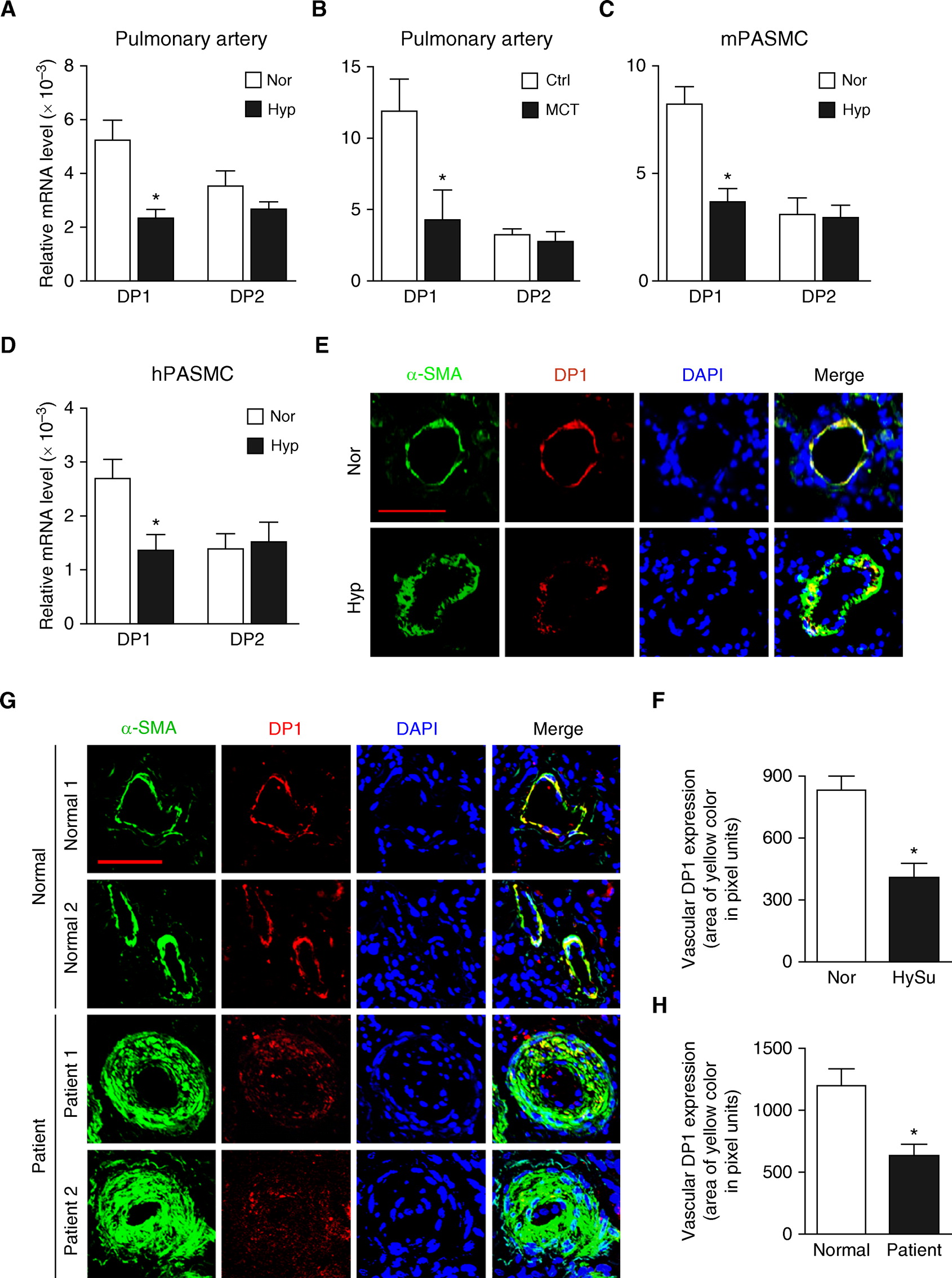
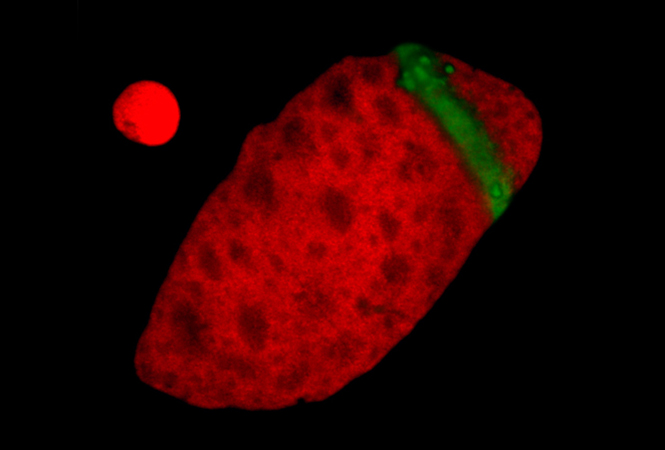
DP1(D 前列腺素受体亚型 1)在肺动脉平滑肌细胞中因缺氧而下调
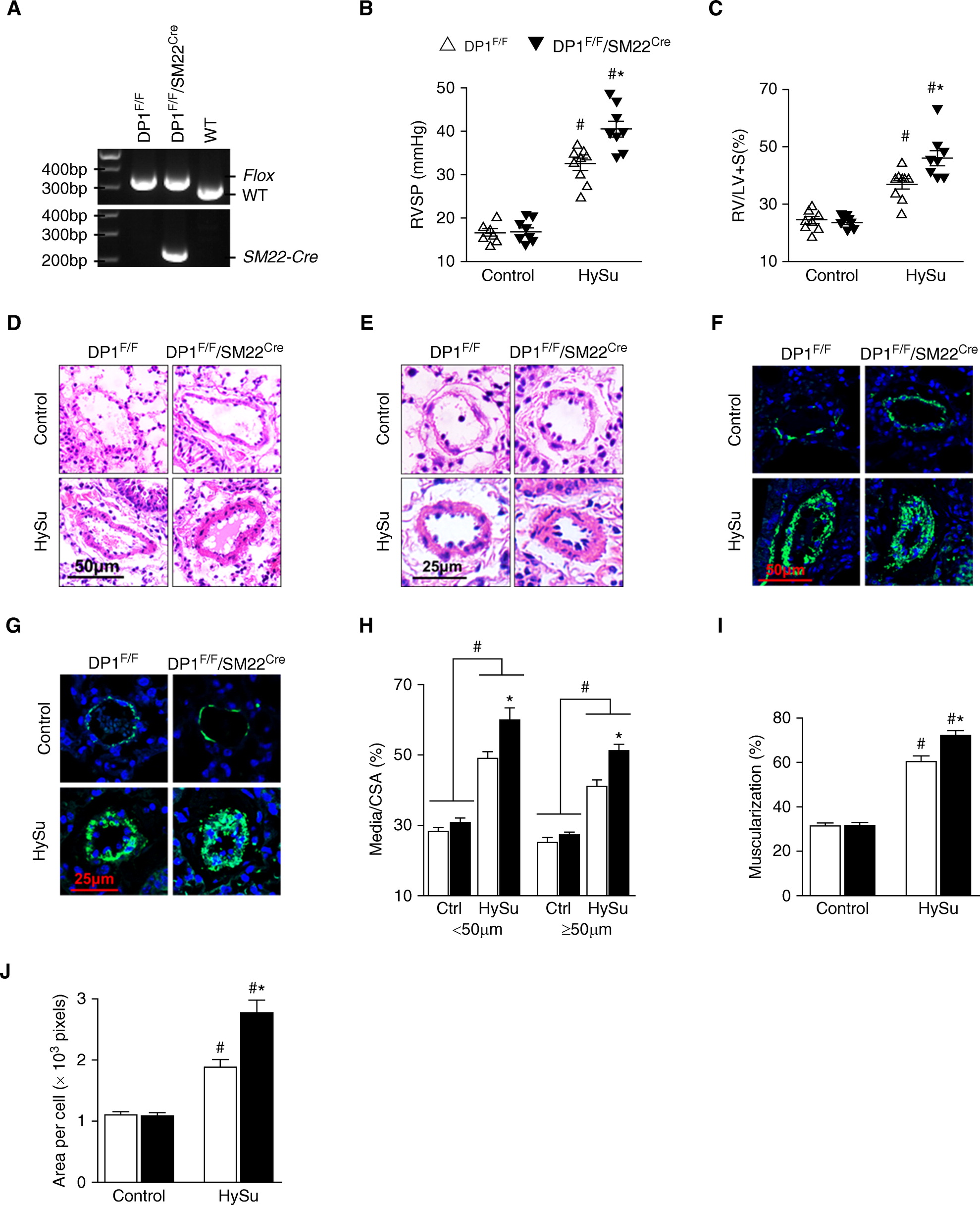
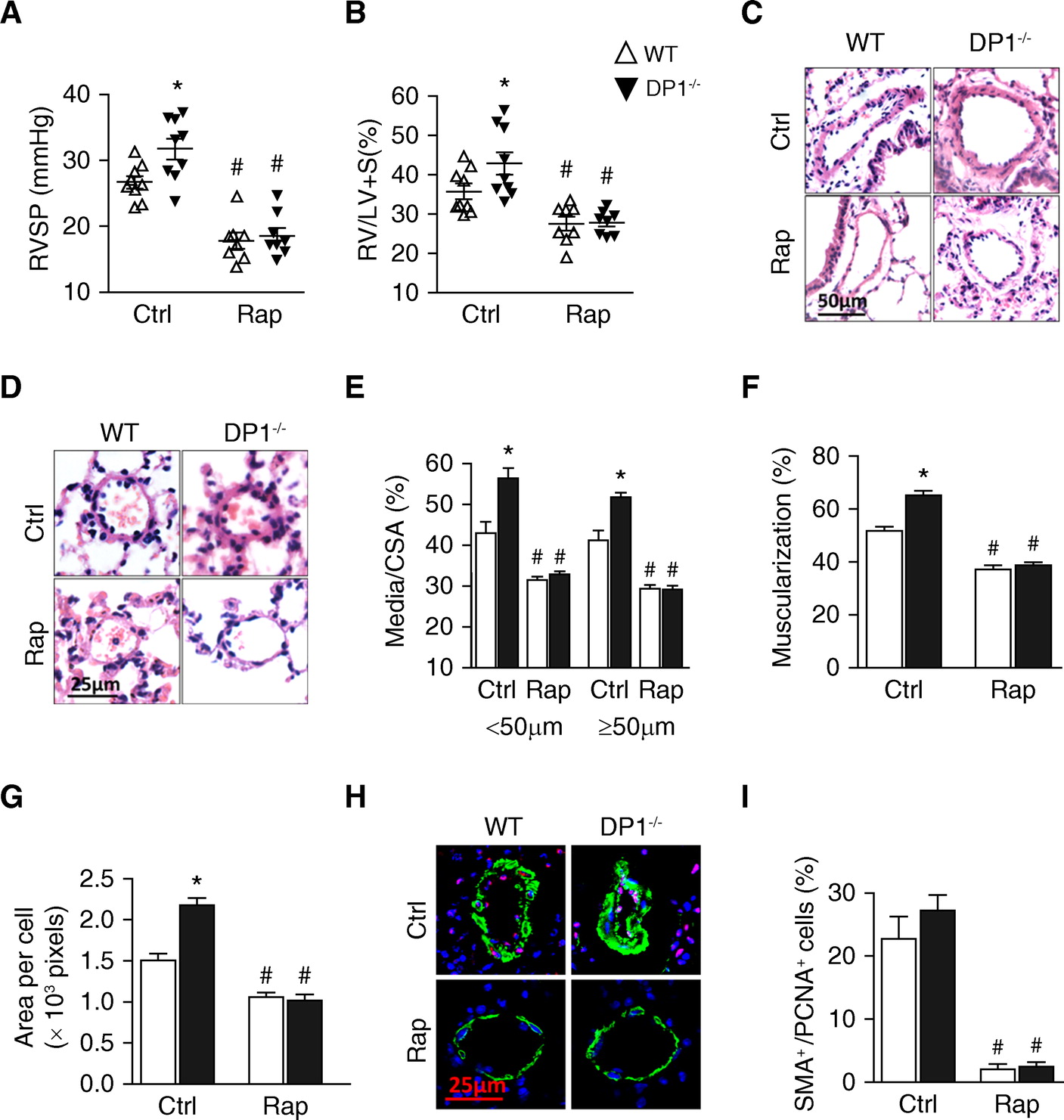
血管平滑肌细胞特异性 DP1(D 前列腺素受体亚型 1)缺失加剧小鼠缺氧诱导的肺动脉高压和肺动脉重塑
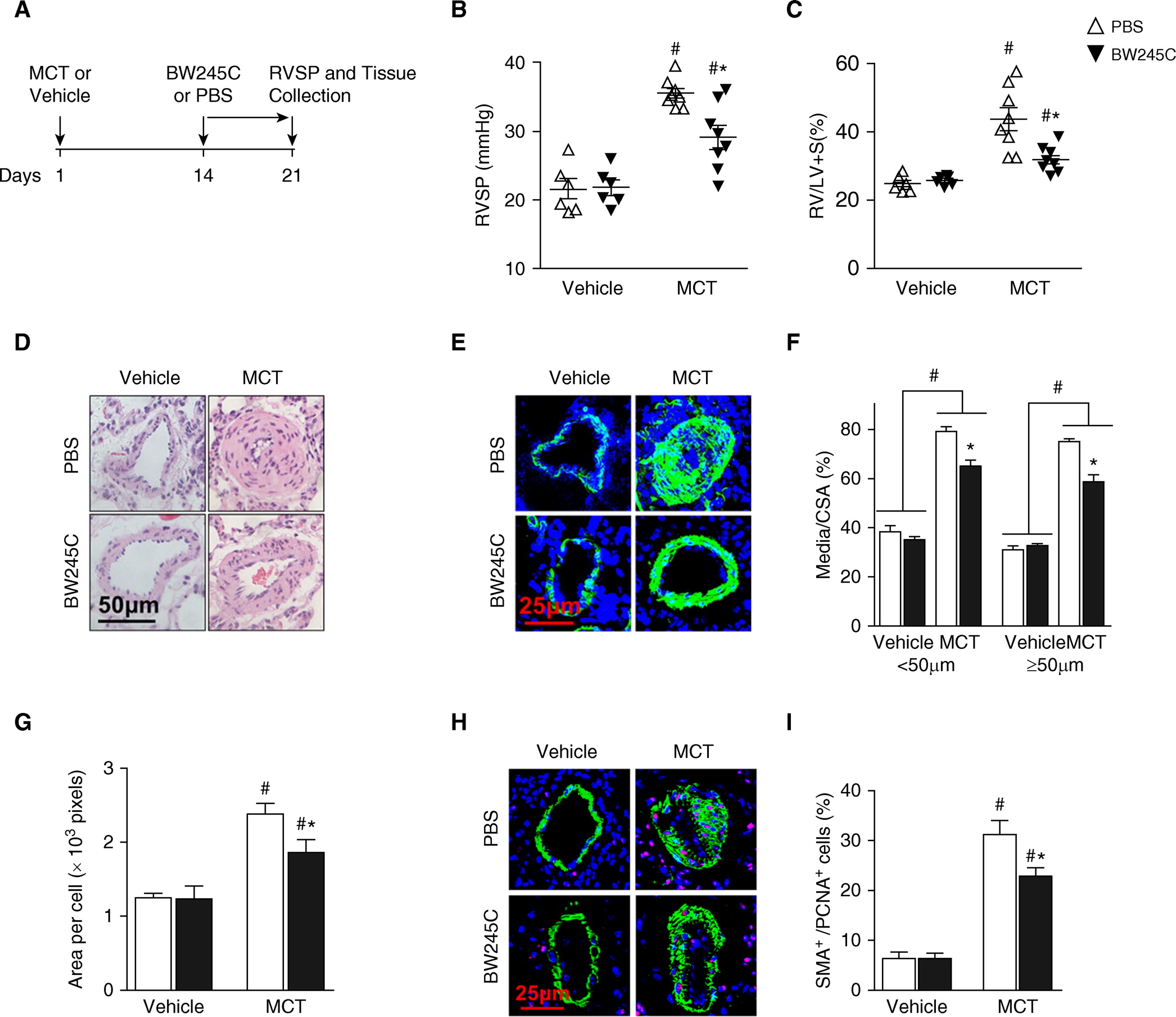
DP1(D 前列腺素受体亚型 1)激动剂治疗抑制野百合碱 (MCT) 诱导的大鼠肺动脉高压的进展
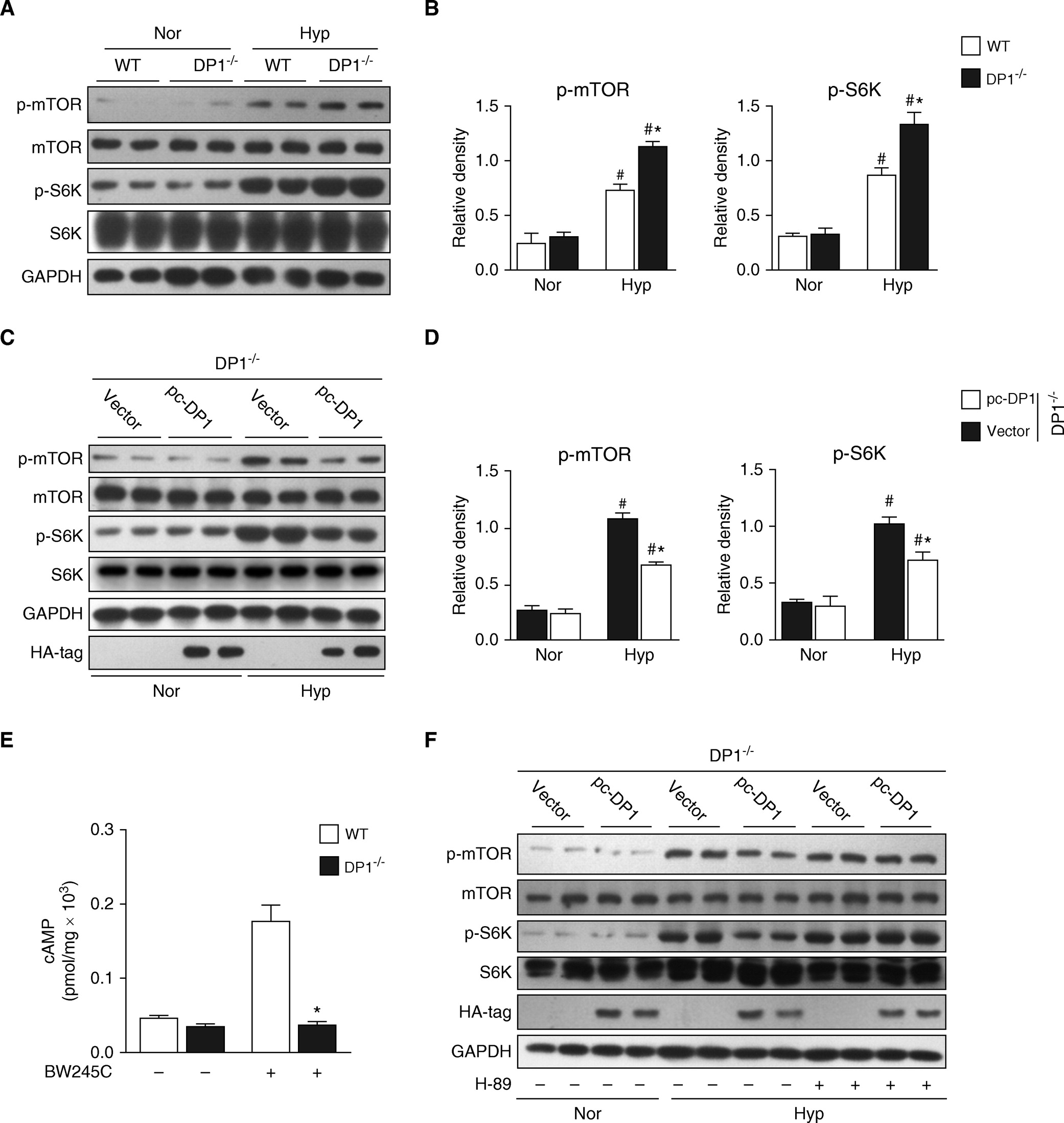
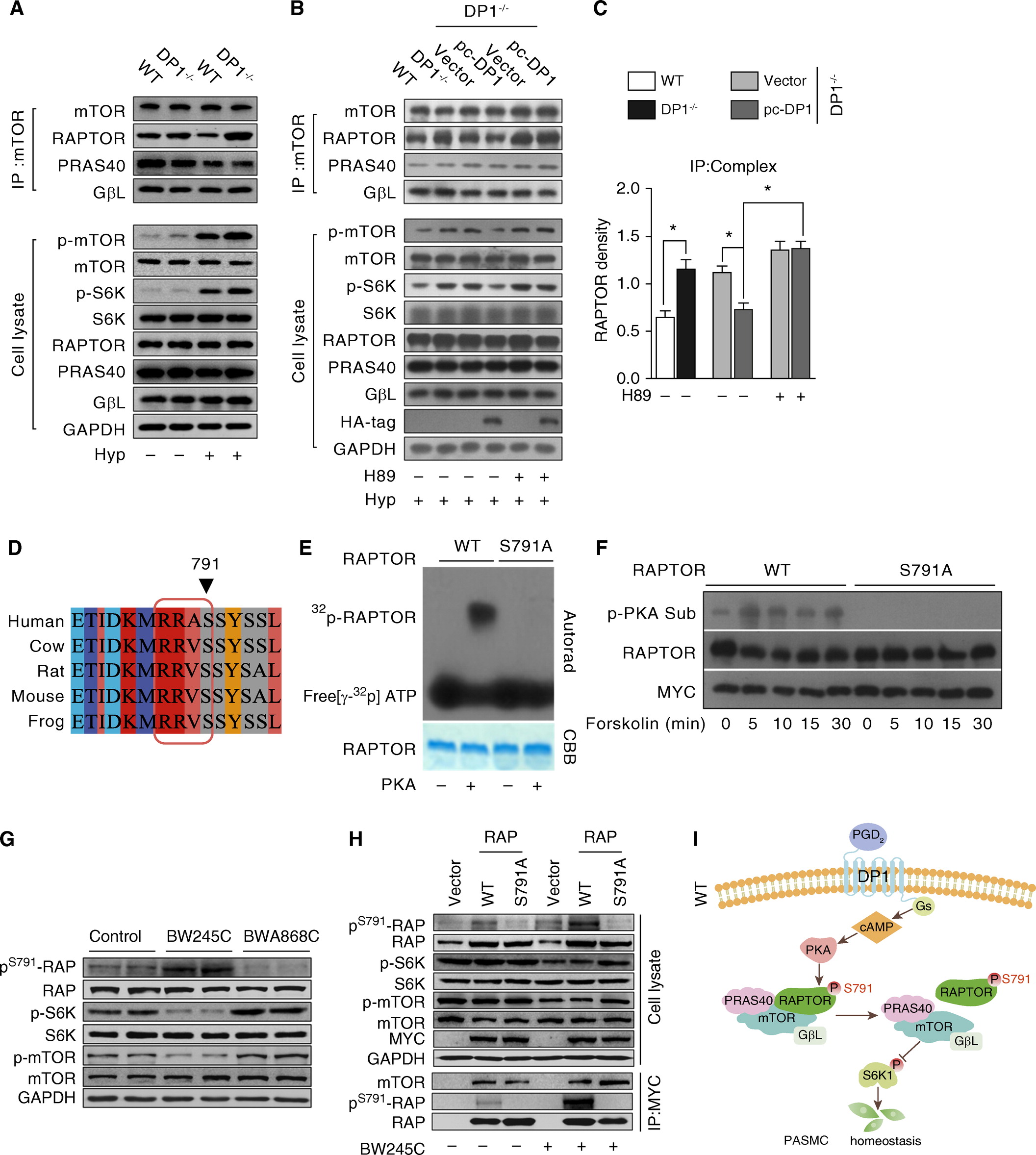
 缺氧条件下,DP1(D 类前列腺素受体亚型 1)缺陷通过 cAMP/PKA(蛋白激酶 A)信号传导增强肺动脉平滑肌细胞中的 mTOR活性
缺氧条件下,DP1(D 类前列腺素受体亚型 1)缺陷通过 cAMP/PKA(蛋白激酶 A)信号传导增强肺动脉平滑肌细胞中的 mTOR活性
mTOR(哺乳动物雷帕霉素靶点)抑制可减轻缺氧暴露的 DP1-/- 小鼠的肺动脉高压恶化
DP1缺陷通过 PKA(蛋白激酶 A)诱导raptor与 mTORC1 分离,增强了缺氧 (Hyp) 处理的鼠肺动脉平滑肌细胞中mTORC1的活性
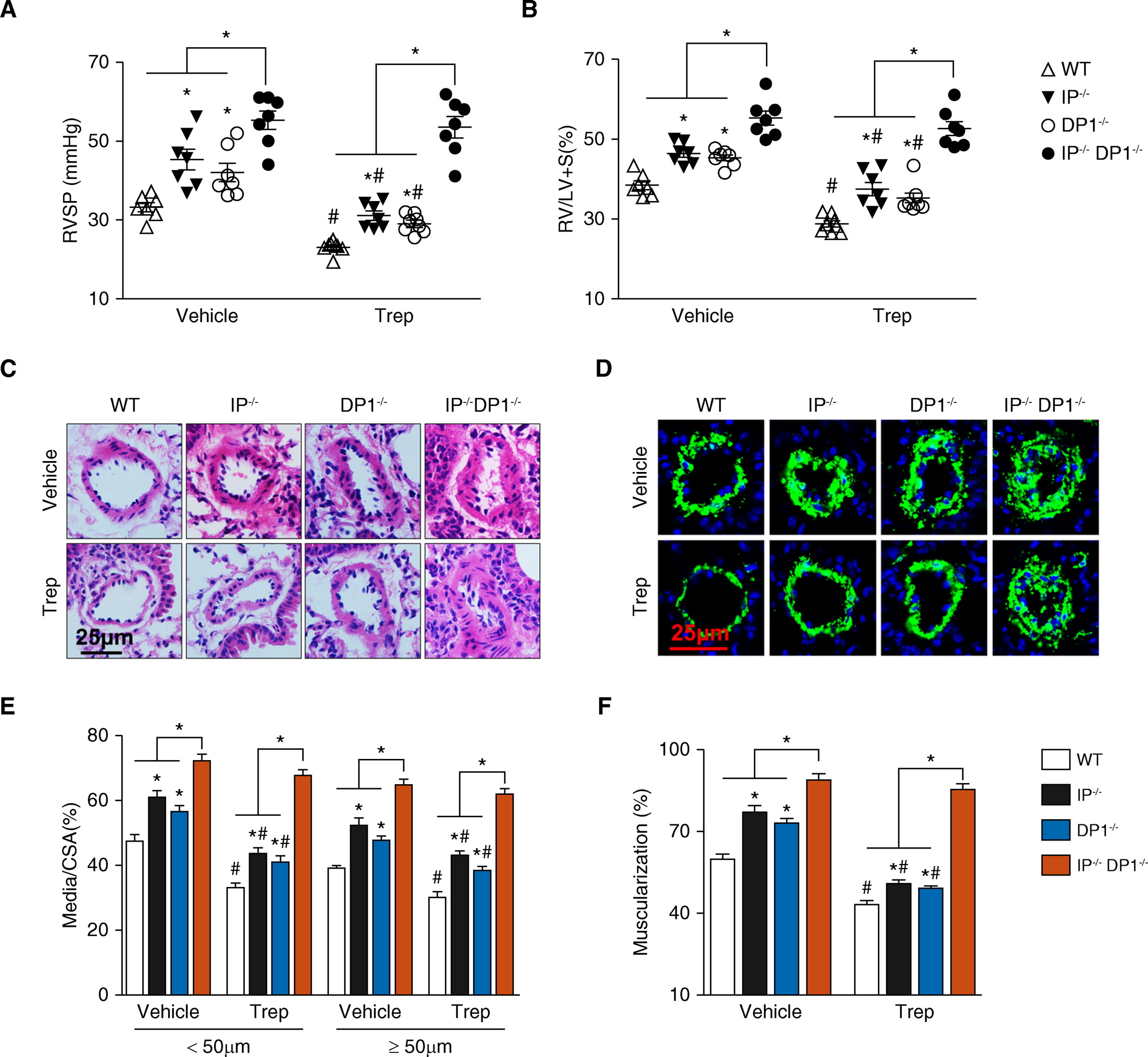
Treprostinil (Trep) 通过激活 DP1和前列腺素 I2 (IP) 受体来防止小鼠缺氧/SU5416 (HySu) 诱导的肺动脉高压
研究结论:
在这项研究中,数据证明了在各种 PAH 动物模型和特发性 PAH 患者的肺动脉中 DP1 表达下调。 DP1 受体的消融加剧了缺氧诱导的 PAH,并通过激活 mTORC1(雷帕霉素复合物 1 的哺乳动物靶标)信号增强了小鼠的肺动脉重塑。 DP1 激活促进了 mTORC1 解离,并通过 Ser791 处的 PKA(蛋白激酶 A)依赖性raptor磷酸化抑制了肺动脉平滑肌细胞中的 mTORC1 活性。 该研究还发现曲前列素部分通过 DP1 受体对小鼠的 PAH 产生治疗作用。DP1 激活通过 PKA 介导的raptor与 mTORC1 的分离减弱了缺氧诱导的肺动脉重塑和肺动脉高压。这些结果表明 DP1 受体可以作为 PAH 管理的治疗靶点。
文章出处:
He Y, Zuo C, Jia D, Bai P, Kong D, Chen D, Liu G, Li J, Wang Y, Chen G, Yan S, Xiao B, Zhang J, Piao L, Li Y, Deng Y, Li B, Roux PP, Andreasson KI, Breyer RM, Su Y, Wang J, Lyu A, Shen Y, Yu Y. Loss of DP1 Aggravates Vascular Remodeling in Pulmonary Arterial Hypertension via mTORC1 Signaling. Am J Respir Crit Care Med. 2020 May 15;201(10):1263-1276. doi: 10.1164/rccm.201911-2137OC. PMID: 31917615; PMCID: PMC7233340.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#血管重构#
38
#RCC#
28
#动脉高压#
24
谢谢分享
66
谢谢分享
63
#mTORC1#
31