BMJ:儿童SARS-CoV-2血清流行的聚集性和纵向变化——对55所学校的前瞻性队列研究
2021-03-18 MedSci原创 MedSci原创
尽管SARS-CoV-2在社区中中度至高传播期间整体血清流行率有所上升,但随着2020年8月学校开学并采取了一些预防措施,只有少数班级出现了聚集性血清阳性儿童。
Pixabay.com
学校儿童在传播新冠病毒(SARS-CoV-2)感染中的作用仍是一个有争议的问题。儿童,特别是青少年的感染率可能与成人一样高,但儿童很少出现明显的临床表现或严重的健康后果。然而,关于无症状或症状很少的儿童感染率以及在学校的潜在传播的争论仍在继续。许多国家在2020年上半年关闭了学校以遏制这一流行病,截至20207年4月,这导致多达172个国家15亿学生的教育中断;2021年2月2日,仍有2亿多学生受到学校关闭的影响。
近日,BMJ上发表了一篇相关研究,这项研究的目的是估计个人、学校、地区和州各级血清流行率的纵向变化;计算诊断为SARS-CoV-2感染的儿童与血清阳性儿童的比率;评估血清阳性与报告症状的相关性;确定聚集的频率对班级和学校内血清阳性的儿童进行调查;并调查观察到的集群的潜在原因。
2020年秋季,瑞士是欧洲第二波SARS-CoV-2大流行最严重的国家之一。保持学校开放为研究SARS-CoV-2感染提供了一个中等到高暴露的环境。随机抽取学校和班级的儿童,按地区分层,进行SARS-CoV-2血清学检测。父母完成了关于社会人口和健康相关问题的问卷调查。纳入的55所学校有275个班;2020年6月至7月有2603名儿童参加,2020年10月至11月有2552名儿童参加(年龄范围6-16岁)。
6月至7月,在2496名有血清学结果的儿童中,有74名呈血清学阳性;10月至11月,这一数字增加到2503名儿童中的173名。在以前没有血清阳性的儿童中,SARS-CoV-2血清总流行率在夏季为2.4%(95%可信区间为1.4%至3.6%),在深秋为4.5%(3.2%至6.0%),因此,估计有7.8%(6.2%至9.5%)的儿童血清呈阳性。不同地区的血清流行率不同(秋季为1.7-15.0%)。低、中、高年级儿童(分别为6-9岁、9-13岁和12-16岁)之间无显著差异。
2223名儿童在两轮检测中都进行了血清学检查,其中28/70(40%)先前血清阳性者转为血清阴性,109/2153(5%)先前血清阴性者转为血清阳性。自夏季以来,22%的血清阴性儿童和29%的新血清阳性儿童出现了症状。在2020年7月至11月期间,被诊断为SARS-CoV-2感染的儿童与血清阳性儿童的比例为1比8。
在55所学校中的47所学校和275个班级中的90个班级中,至少发现了一名新的血清阳性儿童。在130个参与率高的班级中,73个班级(56%)未发现血清阳性儿童,50个班级(38%)有1至2名儿童血清阳性,7个班级(5%)至少有3名儿童血清阳性。在多水平logistic回归模型中,班级水平和学校水平分别解释了24%和8%的血清阳性变异。
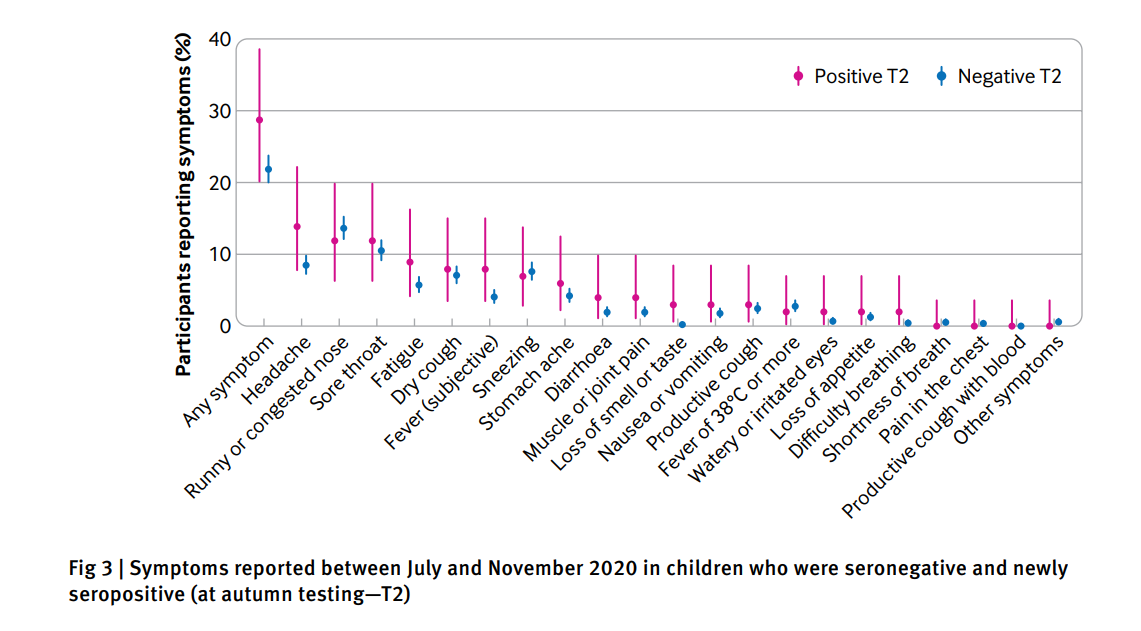
2020年7月至11月在血清阴性和新血清阳性(秋季试验T2)儿童中报告的症状

在至少有5名儿童和50%或以上儿童接受测试的班级中,T1血清阳性和T2新血清阳性儿童的分布
本研究通过随机选取的具有代表性的纵向人群队列,对SARS-CoV-2在学校的传播和流行情况提供了独特的见解。其他大多数关于学校中SARS-CoV-2感染的研究集中在追踪指示病例(1128例,因此可能失踪的不明病例)。其他研究依赖于确诊的SARS-CoV-2感染的流行率来评估学校开放期间儿童暴发的频率和感染风险。一些研究试图评估关闭和开放学校对报告的SARS-CoV-2感染和死亡的总体影响。
尽管SARS-CoV-2在社区中中度至高传播期间整体血清流行率有所上升,但随着2020年8月学校开学并采取了一些预防措施,只有少数班级出现了聚集性血清阳性儿童。这些发现是否会随着SARS-CoV-2的新变种和社区传播的动态水平而改变仍不确定。
参考文献:Agne Ulyte, Thomas Radtke, Irene A Abela, Sarah R Haile, Christoph Berger, Michael Huber, Merle Schanz, Magdalena Schwarzmueller, Alexandra Trkola, Jan Fehr, Milo A Puhan, Susi Kriemler .Clustering and longitudinal change in SARS-CoV-2 seroprevalence in school children in the canton of Zurich, Switzerland: prospective cohort study of 55 schools BMJ 2021; 372 doi: https://doi.org/10.1136/bmj.n616 (Published 17 March 2021)Cite this as: BMJ 2021;372:n616
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#前瞻性队列研究#
48
#BMJ#
27
#前瞻性队列#
34
#SARS-CoV#
31
#前瞻性#
31
#SARS#
27