TRANSFUSION:出血性创伤患者的血小板和红细胞的比率与死亡率的关系:系统评价和荟萃分析
2022-01-15 MedSci原创 MedSci原创
在创伤性出血中,与低血小板:RBC 比率相比,高血小板:RBC 可提高死亡率。高血小板:RBC 比率不影响血栓栓塞或器官衰竭事件的发生率。
不受控制的出血仍然是可预防的受伤后死亡的主要原因之一。这些患者中有 30%–40% 会出现创伤性凝血病 (TIC)。TIC 与早期和晚期死亡率相关,血小板在 TIC 的病理生理学中起重要作用。在创伤性出血中,输血实践已转向更高剂量的血小板和血浆输注。一项系统评价分析研究里,研究人员欲探讨与较低的血小板与红细胞 (RBC) 比值相比,较高的血小板与红细胞 (RBC) 输注比是否可以提高死亡率而不加重器官衰竭。

图1:选取流程流程图
研究人员从Pubmed、Medline 和 Embase 对 1946 年至 2020 年 10 月期间接受血小板输注的出血性创伤患者(年龄≥16 岁)的随机对照试验 (RCT) 进行了筛选。高血小板:红细胞比率被定义为纳入研究中的最高比率. 主要结果是 24 小时死亡率。次要结局是 30 天死亡率、血栓栓塞事件、器官衰竭和凝血功能障碍的纠正。
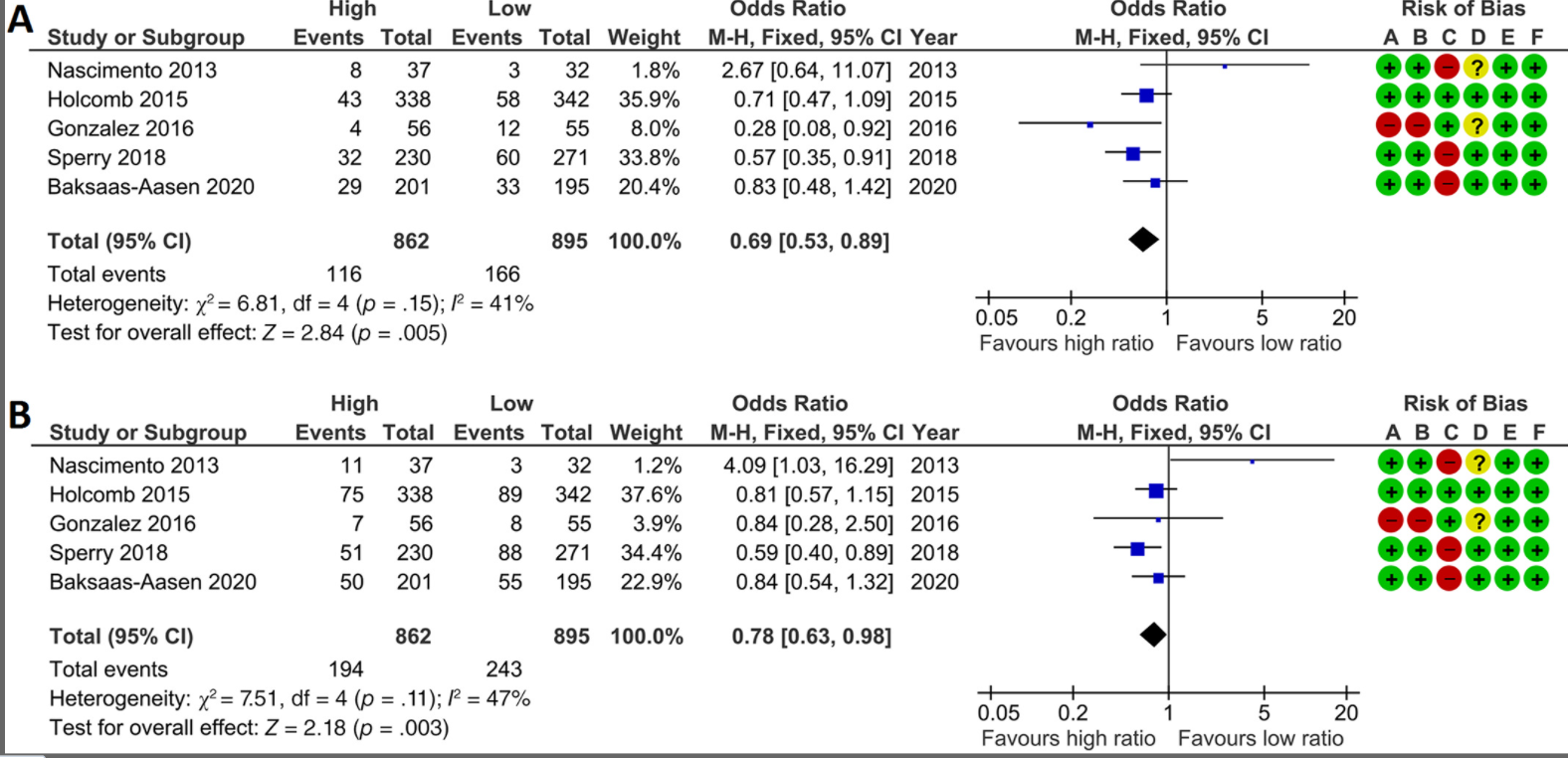
图1:研究的总体质量中等,如图 2所示。由于人员不可能对治疗策略的分配实施盲法,除一项 RCT 外,所有 RCT 均获得高偏倚风险。
一共纳入了五项随机对照试验(n = 1757 名患者)。与低血小板:红细胞比率相比,高血小板:红细胞显着改善了 24 小时死亡率(优势比 [OR] 0.69 [0.53–0.89])和 30 天死亡率(OR 0.78 [0.63–0.98])。在血栓栓塞事件和器官衰竭方面,血小板:红细胞比率组之间没有差异。五项研究报告了凝血障碍的纠正,其中血小板剂量对创伤引起的凝血障碍没有影响。
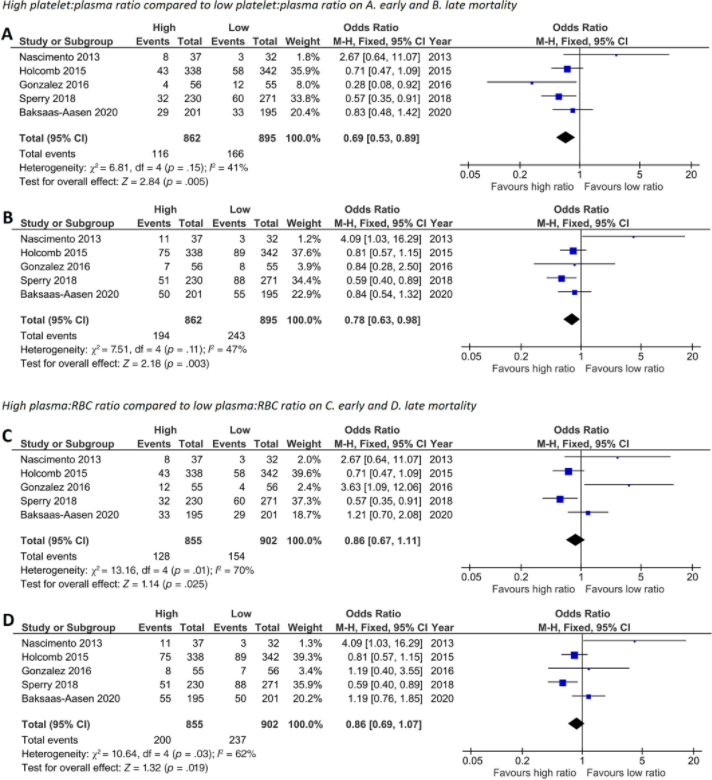
图2:在随机对照试验中,高血小板:血浆,但不高血浆:RBC 比率可提高 24 小时死亡率和 30 天死亡率。(A) 24 小时和 (B) 30 天死亡率的高和低血小板:血浆比值以及 (C) 24 小时和 (D) 30 天死亡率的高和低血浆:RBC 比值的荟萃分析在一片森林里。高比率组的加权平均血小板:血浆比率为 1.08 (SD 0.56),低比率组为 0.65 (0.38)。高比率组的加权平均血浆:RBC 比率为 0.70 (0.34),低比率组为 0.53 (0.30)。事件 = 死亡人数,总数 = 患者总数,高 = 血小板:血浆或血浆:RBC 比率最高的组,低 = 血小板:血浆或血浆:RBC 比率最低的组,MH = Mantel-Haenszel
图3:在随机对照试验中,高血小板:红细胞比率对创伤患者的血栓栓塞事件或器官衰竭没有影响。森林图中表示的 (A) 血栓栓塞事件 (TEE) 和 (B) 多器官功能障碍综合征 (MODS) 的高低血小板:RBC 比率的荟萃分析。高比率组的加权平均血小板:RBC 比率为 1.15 (SD 0.34),低比率组 TEE 为 0.56 (0.15),MODS 为 0.83 (0.56) 和 0.39 (0.27)。事件 = 受影响的患者人数,总数 = 患者总数,高 = 血小板:RBC 比率最高的组,低 = 血小板:RBC 比率最低的组,MH = Mantel-Haenszel
结果提示,与低血小板:红细胞比率相比,高与低的复苏可改善创伤性出血患者的早期和晚期死亡率。高血小板:红细胞比率不影响器官衰竭的发生。血小板:红细胞的最佳比例及其对创伤性出血中血小板功能的影响仍有待确定。
但该系统评价亦存在若干局限性,如计算血小板:红细胞比率的方法导致高比率组和低比率组的输血比率可能重叠,这可能会影响分析。然而,在确定比率时,并非所有研究都报告了血小板产品的类型(单采或混合血沉棕黄层血小板)和接受血小板输注的患者数量,因此无法计算绝对血小板:红细胞比率。此外,如果输血比例存在重叠,高血小板剂量对死亡率的影响可能更大。
原始出处:
Kleinveld DJB, van Amstel RBE, Wirtz MR, Geeraedts LMG, Goslings JC, Hollmann MW, Juffermans NP. Platelet-to-red blood cell ratio and mortality in bleeding trauma patients: A systematic review and meta-analysis. Transfusion. 2021 Jul;61 Suppl 1(Suppl 1):S243-S251. doi: 10.1111/trf.16455. PMID: 34269443; PMCID: PMC8362120.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Transfusion#
52
#TRA#
53
#Fusion#
49
#荟萃分析#
43
#荟萃#
45
#红细胞#
49
#创伤#
45
#评价#
35
学习#学习#
62