Br J Cancer:LIMK2介导的SPOP磷酸化降解促进去势抵抗性前列腺癌的发生发展
2020-12-29 xiaozeng MedSci原创
前列腺癌(PCa)目前仍是泌尿外科癌症中最普遍的类型,在美国,其在男性癌症相关死亡中排名第二。2020年美国约有191,930例新病例和33,330例预测死亡病例。尽管雄激素剥夺疗法可以有效治疗该疾病
前列腺癌(PCa)目前仍是泌尿外科癌症中最普遍的类型,在美国,其在男性癌症相关死亡中排名第二。2020年美国约有191,930例新病例和33,330例预测死亡病例。尽管雄激素剥夺疗法可以有效治疗该疾病,但几乎所有的肿瘤最终都会发展成为致命的去势抵抗性PCa(CRPC)。3,4因此,迫切需要探究CRPC发病的相关分子机制,以鉴定有效的药物靶标。
SPOP作为一种重要的E3泛素连接酶,其可以充当肿瘤抑制因子或肿瘤启动因子。在PCa中,其通过降解几种致癌底物来抑制肿瘤的发生。 SPOP是PCa中出现突变最多的基因(约15%),这些突变使该蛋白无效,并促进了癌症的发生。
而保留了野生型状态SPOP的其余PCa肿瘤仍能够发展为CRPC,说明存在其他重要的调节机制来下调SPOP的表达。既往研究显示,在携带野生型SPOP的前列腺肿瘤中,SPOP的表达水平降低了约94%,然而尚不清楚其下调的相关分子机制。
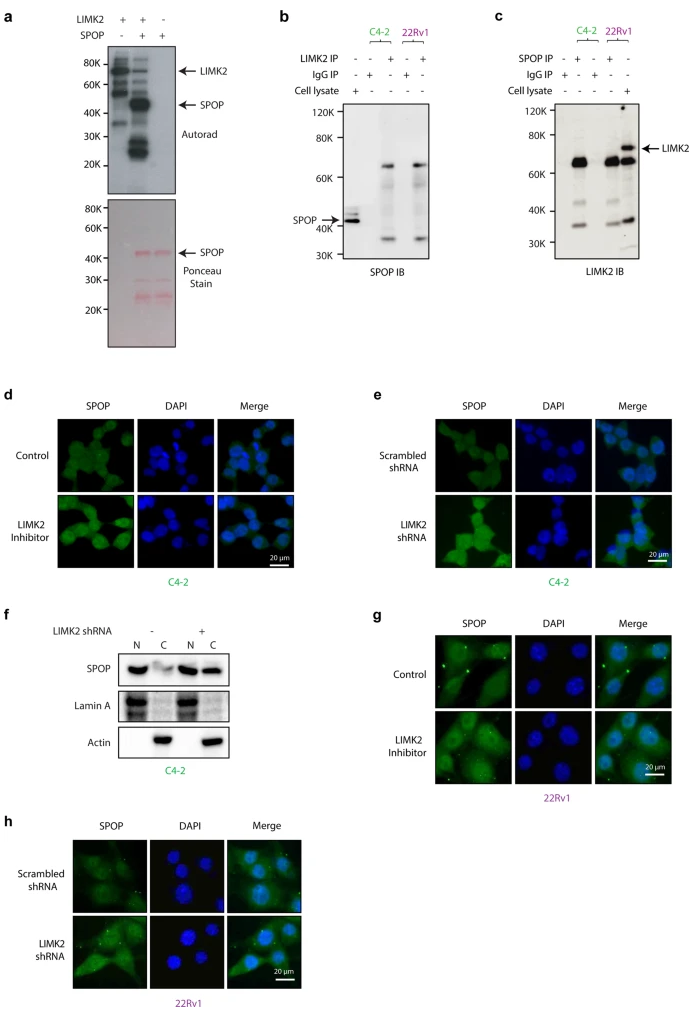
LIMK2直接磷酸化SPOP并调节其核定位
该研究确定了SPOP为LIMK2的直接靶标。并通过多种生化分析方法检测了SPOP和LIMK2之间的相互关系及其致癌作用。同时通过移植瘤实验进一步在在体水平验证了这种关系。
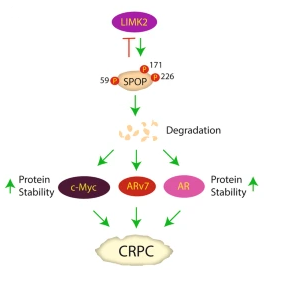
研究人员发现,LIMK2可通过直接磷酸化SPOP的三个位点并降解SPOP,而反过来SPOP能够促进LIMK2的泛素化,从而形成了一个反馈环。SPOP的降解可巩固AR、ARv7和c-Myc的致癌作用。进一步的研究显示,抗磷酸化的SPOP能够完全抑制体内肿瘤的发生,说明LIMK2介导的SPOP降解是PCa发生发展过程中的一个关键事件。
LIMK2-SPOP信号通路影响CRPC发病的相关模型
总而言之,该研究结果显示,携带基因突变SPOP肿瘤患者需要相应的基因治疗策略,而LIMK2-SPOP之间的关系也说明,通过抑制LIMK2维持野生型SPOP或能够抑制该疾病的发生发展。
原始出处:
Nikhil, K., Haymour, H.S., Kamra, M. et al. Phosphorylation-dependent regulation of SPOP by LIMK2 promotes castration-resistant prostate cancer. Br J Cancer (14 December 2020).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













学到了
54
#SPOP#
39
#抗性#
40
学习了
65
#发生发展#
31
#去势抵抗性前列腺癌#
29
好文章!
91
更新及时,很好的课程,继续努力💪
73
学习了
59
LIMK2介导的SPOP磷酸化降解促进去势抵抗性前列腺癌的发生发展
52