BMJ:信迪利单抗联合化疗一线治疗可显著延长晚期/转移性食管鳞癌患者的生存期
2022-04-27 Nebula MedSci原创 发表于威斯康星
信迪利单抗联合化疗作为晚期或转移性食管鳞癌患者的一线治疗可显著延长其总生存期和无进展生存期
食管鳞状细胞癌是食管癌的主要亚型,约占全部食管癌的90%。我国是食管癌高发的国家,食管鳞状细胞癌患者数量占全球的一半以上。
目前,晚期或转移性食管鳞癌患者的一线治疗仅限于以铂为基础的化疗。本研究旨在评估信迪利单抗 vs 安慰剂 联合化疗 (顺铂+紫杉醇或顺铂+5-氟尿嘧啶) 作为不可切除的局部晚期、复发或转移性食管鳞癌的一线治疗的效果和安全性。
这是一项在我国 66个地点和国外 13 个地点开展的多中心、随机、双盲的3期试验,招募了年满18岁的未接受过全身治疗的晚期或转移性食管鳞癌患者。受试患者被随机(1:1)分成两组,接受信迪利单抗或安慰剂联合化疗治疗,1次/3周。主要终点是总人群和PD-L1表达联合阳性评分≥10的患者的总生存期。
2018年12月14日-2021年4月9日期间,共招募了659位患者被随机分至两组:信迪利单抗组 327位,安慰剂组 332位。616位(93%)患者接受了信迪利单抗或安慰剂+顺铂和紫杉醇治疗,43位(7%)患者接受了信迪利单抗或安慰剂+顺铂和5-氟尿嘧啶治疗。
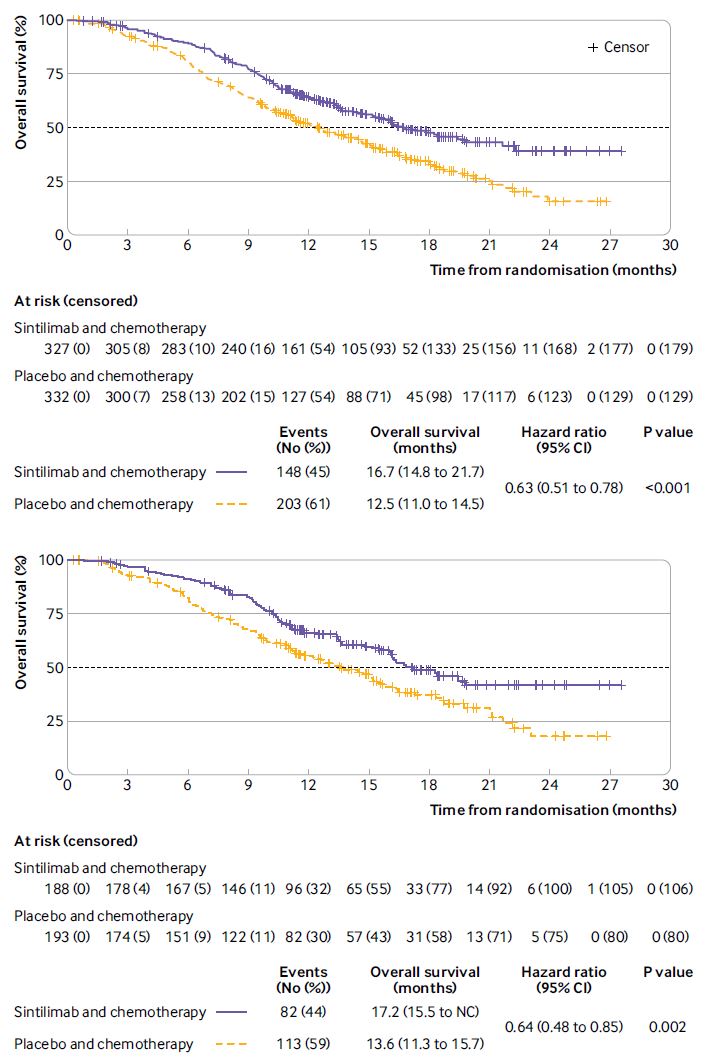
在总人群和PD-L1表达联合阳性评分≥10的患者中,两组的总生存率
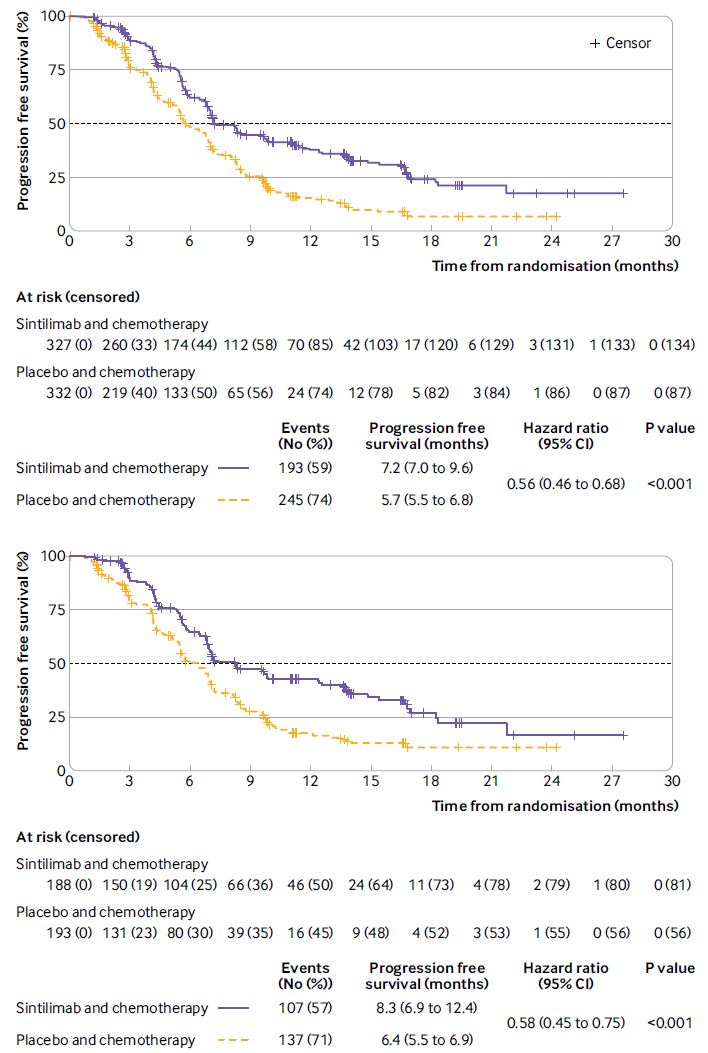
无论是在总人群还是在PD-L1表达联合阳性评分≥10的患者中,与安慰剂组相比,信迪利单抗组患者的总生存期均更长(中位总生存期:16.7 vs 12.5个月,风险比 0.63,p<0.001[总人群];17.2 vs 13.6个月,0.64,p=0.002[PD-L1表达联合阳性评分≥10])。与安慰剂组相比,信迪利单抗联合化疗还可显著延长所有患者和PD-L1表达联合阳性评分≥10的患者的无进展生存期(7.2 vs 5.7个月,0.56,p<0.001; 8.3 vs 6.4个月,0.58,p<0.001)。
在总人群和PD-L1表达联合阳性评分≥10的患者中,两组的无进展生存率
信迪利单抗组327位患者中有321位(98%)经历了治疗相关的不良反应,而安慰剂组332位患者中有326位(98%)。信迪利单抗组和安慰剂组分别有60%(196/327)和55%(181/332)的患者经历了3级及以上的治疗相关的不良反应。
综上,与安慰剂联合化疗相比,信迪利单抗联合化疗作为晚期或转移性食管鳞癌患者的一线治疗可显著延长其总生存期和无进展生存期。
原始出处:
Lu Zhihao,Wang Junye,Shu Yongqian et al. Sintilimab versus placebo in combination with chemotherapy as first line treatment for locally advanced or metastatic oesophageal squamous cell carcinoma (ORIENT-15): multicentre, randomised, double blind, phase 3 trial.[J] .BMJ, 2022, 377: e068714.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#BMJ#
52
#鳞癌患者#
43
#生存期#
57
#转移性#
52
#联合化疗#
58
#食管#
50
#鳞癌#
46
@
52