Liver Int:在急性肝衰竭中由计算机断层扫描确定的肝体积的临床和预后相关性
2018-09-15 MedSci MedSci原创
在ALF/ALI患者中,LV可因病原而显示出不同变化,在疾病预后方面,具有预测作用。在不确定的和由DILI导致的病例中,体积减到小于1000厘米(3)可能表明不可逆的肝损伤和再生失败,并作为作为脑病和死亡发展的早期临床预测因子。
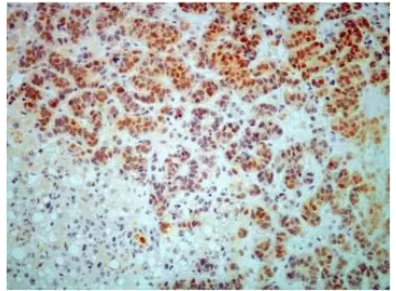
研究背景:肝体积(LV)可从计算机断层扫描(CT)图像的分析中确定,在急性肝损伤(ALI)或急性肝衰竭(ALF)患者中,它可反映肝结构损伤与肝再生的平衡。本研究分析了肝脏体积与肝损伤、肝功能和组织病理学间的相关性,以及预测并发症和死亡的效用。
研究方法:本研究纳入273例ALF/ALI患者。199例患者(73%)存在非对乙酰氨基酚(NA)病因,74例(27%)存在对乙酰氨基酚引起的疾病。LV和预测LV的比例(PLV%)由入院CT成像决定。
研究结果:当病原学组间进行比较时,LV和PLV%显示出明显的变化,包括:因不确定原因而造成的损失 (LV 939 cm3 [IQR 680-1259], PLV% 56% [42-84])和 Budd-Chiari 综合症的增加 (1891 cm3 [1601-2094], 121% [111-131])。LV和PLV较低的患者中,患者疾病进展到高危险水平脑病更为常见。小于1000cm3的阈值,确定NA患者发病前5天的特异性为93%(95%CI 83-98)和优势比为10.6(3.3-34.5);在NA-药物诱发(DILI)或不确定病因的患者中,死亡风险的特异性为91%(71-99)和敏感性为63%(50-75)。
研究结论:在ALF/ALI患者中,LV可因病原而显示出不同变化,在疾病预后方面,具有预测作用。在不确定的和由DILI导致的病例中,体积减到小于1000厘米(3)可能表明不可逆的肝损伤和再生失败,并作为作为脑病和死亡发展的早期临床预测因子。
原始出处
Zabron A, Quaglia A, Fatourou E, et al. Clinical and prognostic associations of liver volume determined by computed tomography in acute liver failure. Liver Int, 2018, 38(9), 1592-1601.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#肝衰#
24
#相关性#
31
#计算机#
25
#急性肝衰竭#
32
嗯嗯,学习了。
56