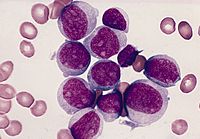
Blood:VEGF,急性淋巴细胞白血病侵入中枢神经系统的新机制
2017-06-01 fengxiangxin MedSci原创
在急性淋巴细胞白血病中,中枢神经系统受累是临床关注的重点。尽管在很多病例中没有检测出中枢神经系统受累,但是对于无复发的幸存者,鞘内注射防治中枢神经系统白血病是必需的。这说明在大部分病人中存在难以构成诊断的亚临床表现
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#淋巴细胞白血病#
40
#神经系统#
39
#淋巴细胞#
29
#VEGF#
28
#中枢神经#
35