Stroke:脑动静脉畸形与静脉内膜增生有关
2017-02-25 xing.T MedSci原创
由此可见,最大静脉管壁厚度增加与较高的大脑动静脉畸形总流量和每引流静脉大脑动静脉畸形流量有关。这一发现表明在静脉内膜增生中有长期较高的大脑动静脉畸形血流流入。
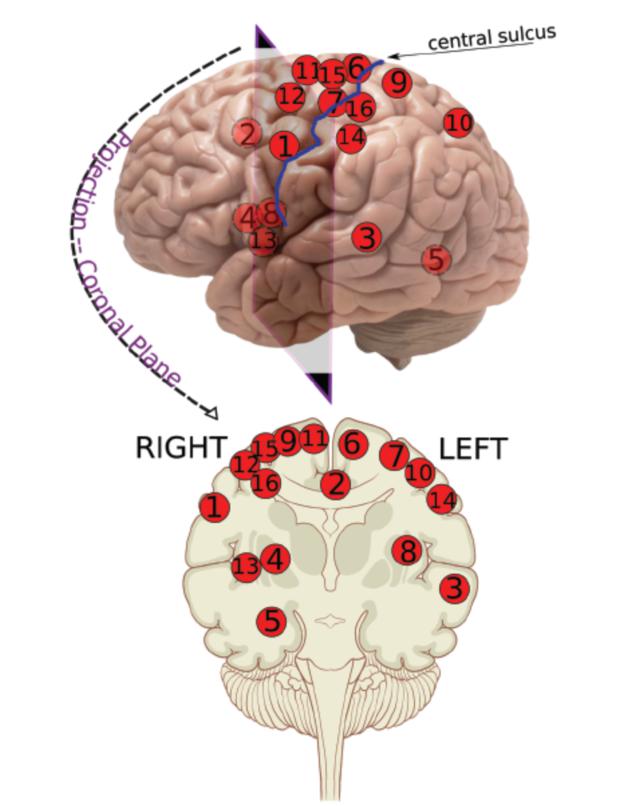
静脉内膜增生以及静脉流出道狭窄的发病机制与大脑动静脉畸形的引流静脉之间是否相关研究人员对其知之甚少。近日,卒中领域权威杂志Stroke上发表了一篇研究文章,研究人员试图确定最大静脉壁的厚度和大脑动静脉畸形血流之间的相关性。
接受了手术切除大脑动静脉畸形并在手术治疗之前使用定量磁共振血管造影对血流量进行了测量的患者被研究人员纳入进行回顾性分析。将患者标本固定子在载波片上,再用弹性蛋白特殊染色进行标本染色。确定周围静脉,并且通过从数字化图像中测定血管最大管壁厚度。研究人员对最大静脉管壁厚度与大脑动静脉畸形血流之间的关系进行了评估。
该研究共纳入了28例大脑动静脉畸形患者。研究人员通过进行Spearman相关分析发现最大静脉管壁的厚度和总的大脑动静脉畸形血流量(ρ=+0.51;P=0.006)、每引流静脉大脑动静脉畸形血流量(ρ=+0.41;P=0.03)和平均巢内血管直径(ρ=+0.39;P=0.04)之间的相关性具有显著的统计学意义。
由此可见,最大静脉管壁厚度增加与较高的大脑动静脉畸形总流量和每引流静脉大脑动静脉畸形流量有关。这一发现表明在静脉内膜增生中有长期较高的大脑动静脉畸形血流流入。
原始出处:
Sophia F. Shakur, et al. Cerebral Arteriovenous Malformation Flow Is Associated With Venous Intimal Hyperplasia.Stroke. 2017.https://doi.org/10.1161/STROKEAHA.116.015666
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#动静脉畸形#
29
#静脉#
26
#内膜#
25
#静脉内膜增生#
27
#畸形#
26