中国急性心梗注册研究(CAMI)分析:预测心梗患者院内死亡风险,GRACE和TIMI评分谁更好?
2019-05-31 朱朱 中国循环杂志
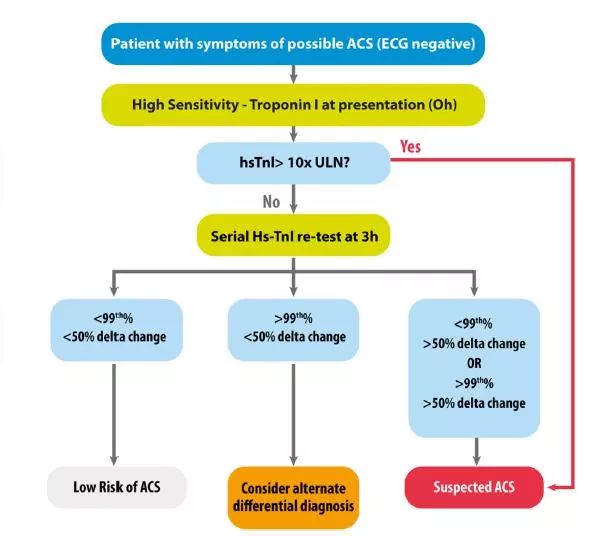
中国急性心肌梗死注册登记(CAMI)研究前期分析结果表明,在预测中国急性ST段抬高型心肌梗死(STEMI)患者院内死亡风险时,TIMI和GRACE两种风险评分价值基本相当。
近期,CAMI研究组最新分析结果提示,对于非ST段抬高型心肌梗死(NSTEMI)患者,这两种风险评分模型对院内死亡风险的评估价值不再一致了,GRACE评分要明显优于TIMI评分。
受试者工作特征(ROC)曲线分析显示,TIMI评分和GRACE评分对中国NSTEMI患者院内死亡率预测价值的曲线下面积分别为0.559和0.793(P<0.001)。
GRACE评分也并非专门针对NSTEMI患者,可用于各种类型的急性冠脉综合征,包括 STEMI和NSTEMI,而且评分所需要的某些变量在入院当时可能无法获得。
因此,还需要探索、寻找更简便、更适合预测中国急性心梗患者预后的评分体系。
研究者对CAMI研究中来自全国31个省、市和自治区107家医院的5 896例NSTEMI患者数据进行了分析。
结果显示,NSTEMI患者平均住院10天,院内死亡率为6%。68.2%为男性,平均年龄为65.4岁。
所有患者中,3.6%发生过院前心脏骤停,仅11.0%接受再灌注治疗,再灌注治疗平均时间为529.5 min,其中10.9%接受急诊经皮冠状动脉介入治疗,0.1%接受急诊冠状动脉旁路移植术。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#注册研究#
35
#心梗患者#
36
#院内死亡#
38
#ACE#
32
#CAM#
33
#死亡风险#
34
#急性心梗#
27
#注册#
35