NAT COMMUN:HER2 CAR T治疗转移性横纹肌肉瘤患儿后的肿瘤反应和内源性免疫反应性
2020-07-16 MedSci原创 MedSci原创
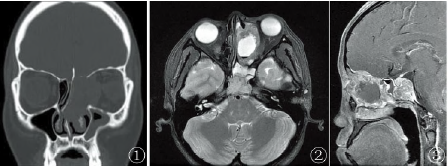
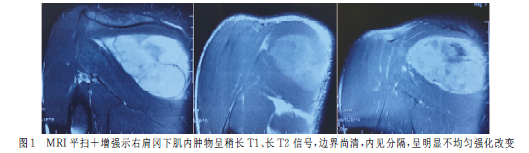
在这里,研究人员分析了一名难治性骨髓转移性横纹肌肉瘤患儿对自体HER2 CAR T细胞的反应。
目前,难治性转移性横纹肌肉瘤基本无法治愈。
在这里,研究人员分析了一名难治性骨髓转移性横纹肌肉瘤患儿对自体HER2 CAR T细胞的反应。
在淋巴清扫化疗后给予三个周期的HER2 CAR T细胞,诱导缓解,并在没有淋巴清扫的情况下再输注4次CAR T细胞,巩固缓解。
纵向免疫监测显示T细胞受体重塑,免疫优势克隆和血清自身抗体对致癌信号通路蛋白有反应。
停药6个月后患者骨髓中疾病复发。给与一个周期的淋巴清除和HER2 CAR T细胞后实现第二次缓解。用额外的CAR T细胞输注进行反应巩固,包括给与pembrolizumab以提高其疗效。
这里描述的患者是一项正在进行的I期试验(NCT00902044;活动中,未招募)的参与者,在本报告发表时,已停止T细胞输注20个月,没有发现疾病。
原始出处:
Meenakshi Hegde et al. Tumor response and endogenous immune reactivity after administration of HER2 CAR T cells in a child with metastatic rhabdomyosarcoma, NATURE COMMUNICATIONS (2020).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#内源性#
43
#Nat#
31
#COMMUN#
40
#反应性#
49
666
95
#免疫反应#
36
#转移性#
34