J Clin Oncol.:宫颈癌辅助化疗+手术VS. 放化疗:孰优孰劣?
2018-02-28 慧语 肿瘤资讯
2018年2月《JOURNAL OF CLINICAL ONCOLOGY》杂志在线发表一篇针对IB2- IIB期的宫颈鳞癌患者III期随机对照研究。尽管新辅助化疗加手术是目前临床治疗模式的主流选择,但仍缺乏足够确切的疗效证据。本研究对比了新辅助化疗+根治术与化放疗联合治疗方案的有效性和安全性。
背 景
宫颈癌是全世界的主要公共卫生问题,鳞状细胞癌是最常见的亚型。国际妇产科联盟(FIGO)将IB2 -IVA期的宫颈癌定义为局部晚期。虽然对IB2期或IIA期患者也可以进行根治性手术,但放疗仍然是治疗的主要方式。自从有研究得到“相比于单纯根治性放疗,放疗同时伴随化疗可以提高生存率”的结论后,宫颈癌的治疗模式开始发生转变。从1999年开始,放疗同时使用铂类化疗已成为局部晚期宫颈癌的标准治疗。然而,仍有25%至40%的患者在放化疗后发生复发,且存在治疗相关的早期和长期毒性,因此治疗的方式的改进仍有提高的空间。
新辅助化疗随后进行根治性子宫切除术被认为是有望改善疾病控制和减少毒性的有效治疗手段。宫颈癌对紫杉、铂类等现代化疗方案的反应敏感,且新辅助化疗可以促进局部控制,还可能根除微转移并减少全身衰竭。有研究报道,与放疗相比,新辅助化疗后再手术可以提高生存率,但研究中使用的化疗方案已略显陈旧,单纯的放疗在目前临床中更是较少涉及。因此开展了此项随机对照研究,针对IB2期,IIA期或IIB期鳞癌患者,两种治疗方案(紫杉醇、卡铂的新辅助化疗+根治术 VS 顺铂为基础的放化疗联合)的有效性和安全性。
患者和方法
本研究是一项单中心III期随机对照试验(ClinicalTrials.gov, NCT00193739)。入组条件为年龄在18-65岁的IB2,IIA或IIB期的宫颈癌鳞状细胞癌患者。以分期作为随机分层因素,将受试者按1:1比例随机分配到两个治疗组,治疗方案分别为每3周一次紫杉醇、卡铂新辅助化疗共三个周期,然后进行根治性子宫切除术(NACT+Surgery);或标准放疗同时铂类化疗,每周一次,持续5周(CTRT)。NACT+Surgery组患者术后可根据需要进行辅助放疗或化放疗。主要研究终点是无疾病生存率(DFS),定义为无复发或死亡的生存。次要研究终点包括总体生存率OS和毒性。
结 果
在2003年9月至2015年2月期间,共有635名患者进行了随机,其中633名被纳入最终分析,包括NACT+Surgery 组316名患者和CTRT组317名患者。中位随访时间为58.5个月,NACT+Surgery组的5年DFS为69.3%,CTRT组为76.7%(HR=1.38;95%CI:1.02-1.87,P = 0.038,图1A),两组的5年OS分别为75.4%和74.7%(HR=1.025; 95%CI:0.752-1.398; P = 0.87,图1B)。两组(NACT+Surgery VS. CTRT)24个月或治疗后迟发的毒性包括直肠(分别为2.2%VS. 3.5%),膀胱(分别为1.6%VS. 3.5%)和阴道(分别为12.0% VS. 25.6%)。
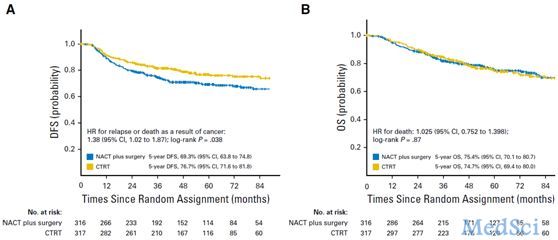
图1 两组患者的DFS和OS生存曲线
结 论
此研究为局部晚期宫颈癌的治疗提供了有力的证据,首次回答了长期尚未有明确答案的重要临床问题。与新辅助化疗+手术相比,以铂类为基础的同步放化疗可以取得更好的DFS。
原始出处:
Sudeep Gupta, Amita Maheshwari, Pallavi Parab,et al.Neoadjuvant Chemotherapy Followed by Radical Surgery Versus Concomitant Chemotherapy and Radiotherapy in Patients With Stage IB2, IIA, or IIB Squamous Cervical Cancer: A Randomized Controlled Trial. J Clin Oncol. 2018 Feb 12:JCO2017759985. doi: 10.1200/JCO.2017.75.9985.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Oncol#
31
MArk
56
#放化疗#
26
#宫颈#
0