休克抢救,锁骨下静脉穿刺不成功怎么办?
2016-12-25 陈都 凌晓 李小勤 徐峰 苏州大学附属第一医院急诊科 医学界急诊与重症频道
锁骨下静脉置管因其感染发生率低、方便护理、患者舒适性好等优点被较多医生认为是较好的选择。但因其有锁骨遮挡因而不适合超声引导,临床上多采用盲穿法。当操作者经验不足时,盲穿容易造成气胸、血胸等严重并发症,尤其是血胸如不能及时发现并处理将导致灾难性后果。那么有没有更好的选择呢?答案是肯定的。随着床旁超声技术的应用,越来越多的医生发现了超声引导深静脉穿刺更安全、更快速。锁骨下静脉向外延伸过第一肋骨后为腋静
锁骨下静脉置管因其感染发生率低、方便护理、患者舒适性好等优点被较多医生认为是较好的选择。但因其有锁骨遮挡因而不适合超声引导,临床上多采用盲穿法。当操作者经验不足时,盲穿容易造成气胸、血胸等严重并发症,尤其是血胸如不能及时发现并处理将导致灾难性后果。
那么有没有更好的选择呢?答案是肯定的。
随着床旁超声技术的应用,越来越多的医生发现了超声引导深静脉穿刺更安全、更快速。锁骨下静脉向外延伸过第一肋骨后为腋静脉(图1),该静脉管腔粗大且无锁骨遮挡,方便超声扫查。
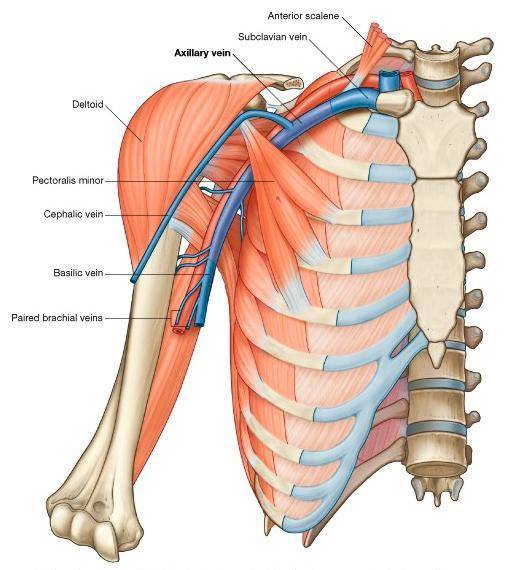
图1 腋静脉解剖:锁骨下静脉向外过第一肋骨延伸为腋静脉(Axillary vein)
① 腋静脉位置较表浅且有肋骨作为屏障,穿刺进入胸腔的可能性极低,不易造成气胸;
② 腋静脉与锁骨下静脉汇合处与动脉距离较远所以误穿动脉几率比较低;
③ 如果误伤腋动脉,因无骨性组织遮挡较锁骨下静脉容易压迫止血;
④ 胸前区皮肤活动少且清洁,便于导管固定及术后护理;
⑤ 住院期间患者可自由活动,导管不易打折且无明显不适。
有研究表明,与锁骨下静脉相比超声引导腋静脉置管能有效提高穿刺成功率、减少穿刺针数、降低并发症的发生率,置管过程中还可观察导管的走向及时纠正导管异位,提高了中心静脉穿刺的安全性和准确性,值得在临床推广应用[1]。我科目前在急诊抢救室常规开展实时超声引导下腋静脉穿刺置管术,取得了较好的临床效果,报道如下:
临床案例
患者中年女性,因“高热两天”入院,入院体温超过 40 度伴意识障碍,外院给予抗感染、补液等治疗后仍有顽固性低血压,入院诊断“脓毒症休克”,立即行实时超声引导下腋静脉穿刺置管术建立深静脉通道(图2),积极抗感染、补液的同时经腋静脉输注激素及血管活性药物。
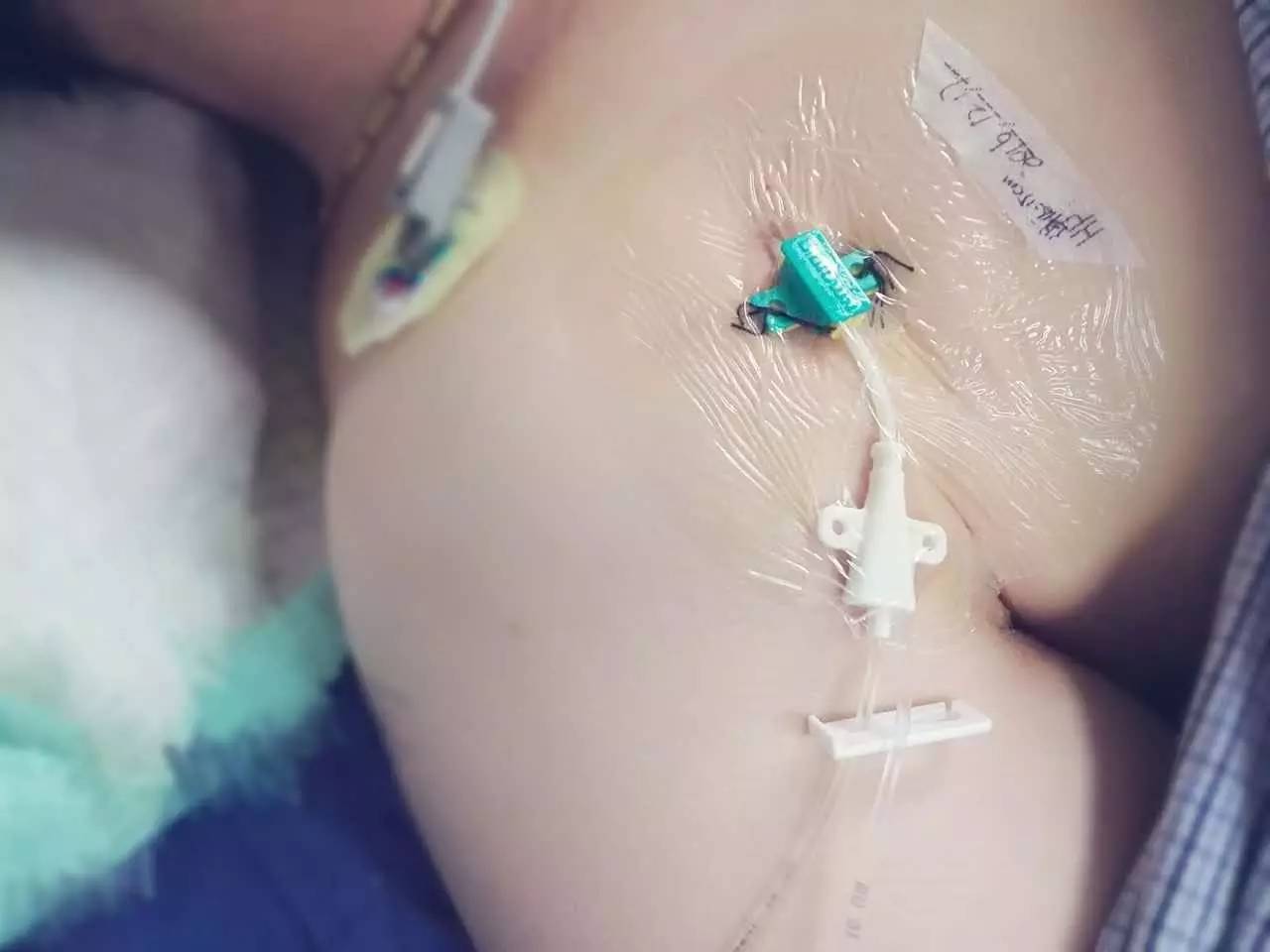
图2 实时超声引导下腋静脉穿刺置管术建立深静脉通道,更安全、更快速
经治疗,患者血压回升,症状好转,意识转清。操作过程中可实时观察穿刺针位置(图3),一次性进入腋静脉,操作过程安全快速(图4)。

图3 采用平面内引导可以观察到穿刺针进入腋静脉全过程
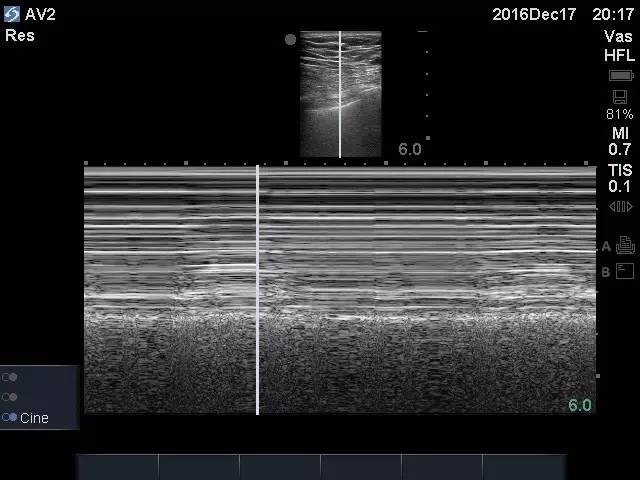
图4 术后对同侧胸腔行M超扫查见肺部呈现“沙滩征”,提示无气胸发生
操作要点
1. 该操作应使用高频线阵探头,术前调节好合适的深度、增益,操作过程中使用无菌套包裹探头。
2. 术前对腋静脉、腋动脉行短轴、长轴等多角度扫查,初步了解其位置、走向及毗邻关系,确定穿刺点。
3. 建议采用平面内引导,以便能实时观察到针尖位置。
4. 探头按压力度适中,过轻易造成图像不佳、探头晃动,过重易压闭腋静脉管腔。
5. 进针过程不必带负压,可在针尖进入血管后再回抽确认。
6. 置入导丝后可再次超声扫查确定导丝走行在腋静脉内。
7. 术毕常规扫查排除气胸及局部血肿。
参考文献
[1] 徐稼轩,王宏志,任宏,等. 超声引导经腋静脉中心静脉置管的应用[J]. 中华临床营养杂志,2013,21(3):163-167.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#休克抢救#
30
#锁骨下#
35
#静脉#
25
#穿刺#
39
#锁骨#
41
#抢救#
32
#静脉穿刺#
39
学习下
51
以前还学习过锁骨下静脉穿刺,挺有意思的。
50
学习了,,,有深入研究嘛?
34