6岁患儿肺动脉高压的原因是……
2017-11-16 熊长明 肺血管病
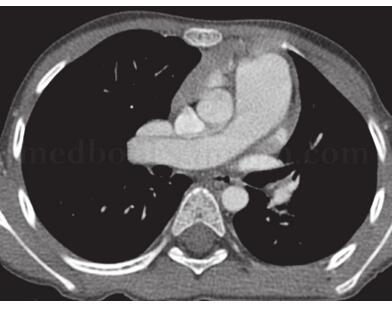
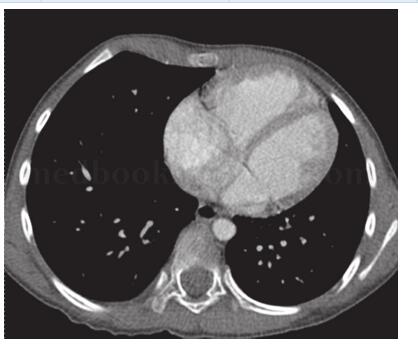
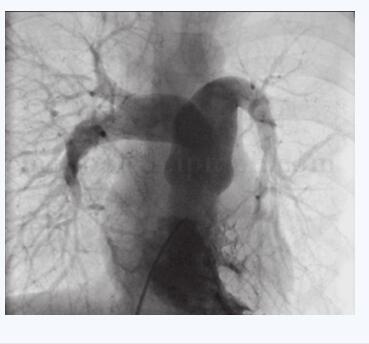
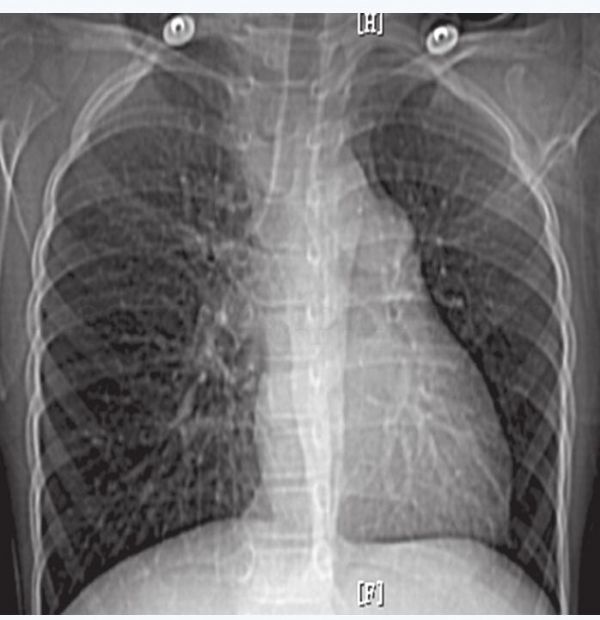
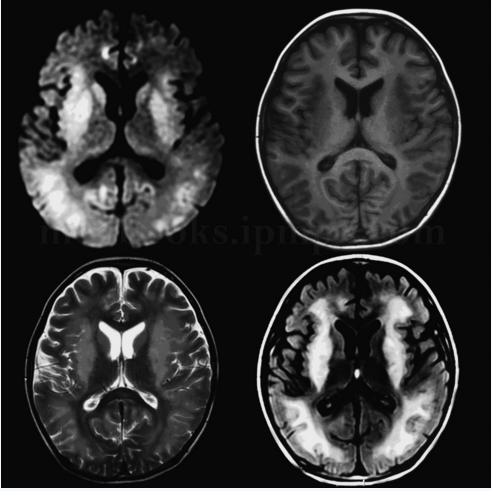
6岁患儿,男,因活动后胸闷、气短1年余入院。患儿1年前出现活动后胸闷、气短,无晕厥、咯血,院外检查发现肺动脉高压。肺动脉高压背后的原因是什么?详见以下病例——



本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#动脉高压#
0
非常好的文章.学习了
70
非常好的文章.学习了
69
好资料学习了!
69
好资料学习了!
58