Dig Liver Dis:回肠储袋-肛门吻合术(IPAA)后发生慢性储袋炎和克罗恩病的危险因素分析
2021-12-31 MedSci原创 MedSci原创
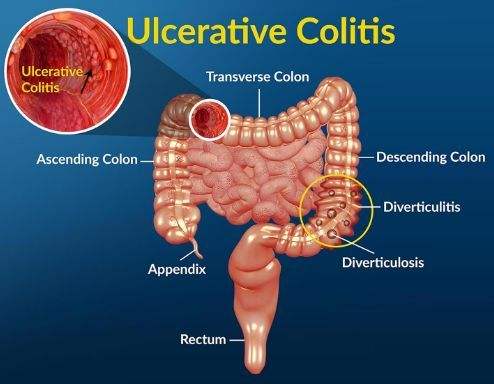
溃疡性结肠炎是一种病因尚不十分清楚的结肠和直肠慢性非特异性炎症性疾病,病变局限于大肠黏膜及黏膜下层。
溃疡性结肠炎(UC)在欧洲影响着大约200万人,在诊断UC后10年,15%的UC患者需要接受手术治疗,修复性直肠切除术与回肠肛门吻合术(IPAA)是UC或未分类的炎症性肠病(IBDU)患者的首选手术方式。然而,有些患者会出现慢性储袋炎症,即慢性储袋炎(CP)或储袋克罗恩病(CDP)。CP和CDP的临床症状相似,主要包括腹泻、直肠出血、腹痛、发烧,腹部绞痛等,并对生活质量产生负面影响。在不同的研究中,出现慢性炎症的患者比例差异很大:CP为11.5%至31.3%,CDP为3.1%至21.3%,本研究的目的是评估IPAA后CP和CDP的发生率,并评估他们的风险因素,鉴别出高风险的患者。

为此,研究人员在巴黎地区的五个三级炎症性肠病诊疗中心进行了一项回顾性研究。将 2011年1月1日至 2019年12月31日期间接受IPAA (J-Pouch)治疗的所有 15 岁以上UC或 IBDU 的连续患者纳入本项研究。所有外科手术均由经验丰富的结直肠外科医生进行。胃肠病学家和外科医生对患者进行了随访,时间直到 2019年12月31日。主要观察结局是CP或CDP的发生。使用多变量和最小绝对收缩和选择算子 (LASSO) Cox 模型寻找风险因素。

本项研究最后包括了 247 名患者。CP 或 CDP 的 5 年累积发生率为 35.3%(95%CI:26.2-43.2)。在多变量分析中,IBDU 的诊断、手术年龄小于 35 岁以及关节外和原发性硬化性胆管炎以外的肠外表现与较高的发病率相关。LASSO 分析确定了这三个预后因素和UC患者关节表现有关。在具有两个或更多预后因素的患者中,5 年累积发生率为 65.2%(95%CI:41.8-79.2)。
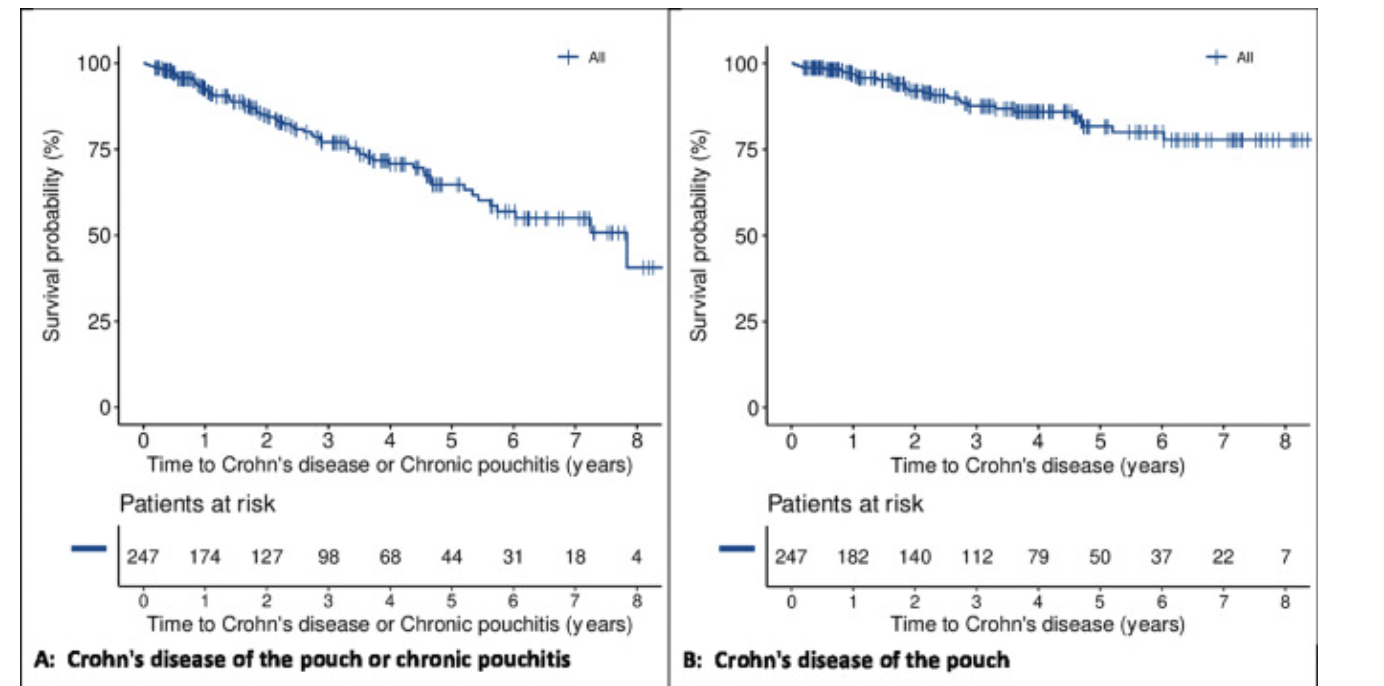
本项研究证实UC患者在接受IPAA术后五年内,大约三分之一的患者会发生 CP 或 CDP。危险因素包括 IBDU、手术年龄小于 35岁、关节表现和其他肠外表现。
原始出处:
ClémentBresteau. Et al. Chronic pouchitis and Crohn's disease of the pouch after ileal pouch-anal anastomosis: Incidence and risk factors. Digestive and Liver Disease.2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#吻合术#
47
#IPAA#
55
#肛门#
43
#Dis#
43
#回肠#
45