JAMA Oncol:非转移去势抵抗性前列腺癌的分子亚型与Apalutamide治疗结果差异的关系
2021-06-25 AlexYang MedSci原创
鉴定预后生物标志物来指导非转移性去势抵抗性前列腺癌(nmCRPC)患者的强化治疗是很有必要的。近期,有研究人员利用随机、双盲、3期SPARTAN试验的存档原发肿瘤样本,调查了分子亚型是否能预测对apa
鉴定预后生物标志物来指导非转移性去势抵抗性前列腺癌(nmCRPC)患者的强化治疗是很有必要的。近期,有研究人员利用随机、双盲、3期SPARTAN试验的存档原发肿瘤样本,调查了分子亚型是否能预测对apalutamide的反应。

在这项队列研究中,包括了233份来自SPARTAN试验中入选的nmCRPC患者的存档样本,使用人类外显子芯片生成了的基因表达数据。分析进行的时间为2018年5月10日至2020年10月15日。
患者随机(2:1)接受apalutamide 240mg/d,同时进行雄性激素阻断疗法(apalutamide+ADT)或安慰剂+ADT。纳入的233名患者的中位年龄为73岁(范围为49-91岁)。在SPARTAN生物标志物子集中,233名患者中有116名(50%)具有较高的GC评分。尽管所有接受apalutamide+ADT的患者的结果都有所改善,但与安慰剂+ADT相比,高GC分数与MFS(危险比[HR],0.21;95%CI,0.11-0.40;P<0.001)、OS(HR,0.52;95%CI,0.29-0.94;P=0.03)和PFS2(HR,0.39;95%CI,0.23-0.67;P=0.001)的最大改善有关。在233名患者中,共有152名(65%)具有基础分子亚型。尽管在安慰剂+ADT组中,管腔亚型与基底亚型患者的MFS、PFS2或OS没有显著差异,但在apalutamide+ADT组中,与基础亚型患者相比,管腔亚型患者的MFS明显延长(apalutamide+ADT:HR,0.40;95%CI,0.18-0.91;P=0.03;安慰剂+ADT:HR,0.66;95%CI,0.33-1.31;P=0.23);OS(apalutamide+ADT:HR,0.50;95%CI,0.25-0.98;P=0.04;安慰剂+ADT:HR,0.78;95%CI,0.38-1.60;P=0.50)和PFS2(apalutamide+ADT:HR,0.71;95%CI,0.42-1.22;P=0.22;安慰剂+ADT。HR, 0.72; 95% CI, 0.38-1.39; P=0.33)也有类似的趋势。在回归分析中,接受apalutamide+ADT的患者的管腔-基底亚型得分与MFS显著相关(HR,2.65;95% CI,1.15-6.08;P=0.02);而在接受安慰剂+ADT的患者中,GC得分与MFS显著相关(HR,2.09;95% CI,1.02-4.27;P=0.04)。
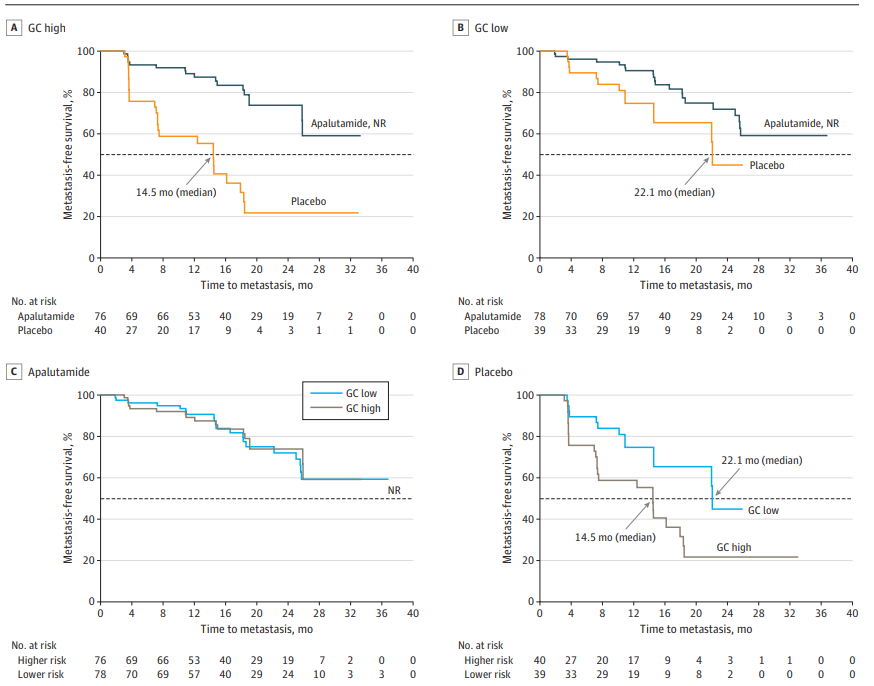
Decipher风险评分与无转移生存(MFS)的相关性
综上所述,GC评分和基底管腔亚型可能是nmCRPC对apalutamide+ADT反应的生物标志物。总体而言,在ADT中加入apalutamide是有益的,其中高风险和管腔亚型似乎受益最大。GC评分可能有助于识别使用apalutamide进行早期强化治疗的患者,而在将新型疗法与apalutamide相结合的试验中,基底-管腔亚型可能是选择进一步强化治疗患者的有益方法。
原始出处:
Felix Y Feng, Shibu Thomas, Fred Saadet al. Association of Molecular Subtypes With Differential Outcome to Apalutamide Treatment in Nonmetastatic Castration-Resistant Prostate Cancer. JAMA Oncol. Jun 2021
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#非转移#
38
#Oncol#
35
#抗性#
40
#APA#
31
#分子亚型#
33
#去势抵抗性前列腺癌#
0
#治疗结果#
38
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
51
谢谢梅斯分享这么多精彩信息
41
前列腺癌相关研究,学习了,谢谢梅斯
55