JAHA:血管周围脂肪中巨噬细胞极化与冠状动脉粥样硬化相关
2022-03-02 MedSci原创 MedSci原创
斑块外周血管周围脂肪组织中的M1巨噬细胞与更高的冠状动脉血栓形成风险相关,并且与斑块进展和不稳定的组织学成分相关。M2巨噬细胞与斑块大小、钙化、坏死含量和外膜层滋养管数量减少相关。
血管周围脂肪组织的炎症可能与动脉粥样硬化有关;然而,冠状动脉血管周围脂肪组织中极化的巨噬细胞与人类动脉粥样硬化成分测量值之间的关系尚未得到充分归纳。

近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,研究人员用血管周围脂肪组织解剖冠状动脉。此外,研究人员评估了动脉阻塞的百分比、内膜中层厚度、纤维帽厚度、斑块成分和血管滋养管的数量,并使用免疫组织化学评估斑块周围和对照血管周围脂肪组织中促炎(M1)和抗炎(M2)巨噬细胞的数量。另一方面,研究人员使用了针对社会人口学和临床变量进行调整后的回归模型进行分析。
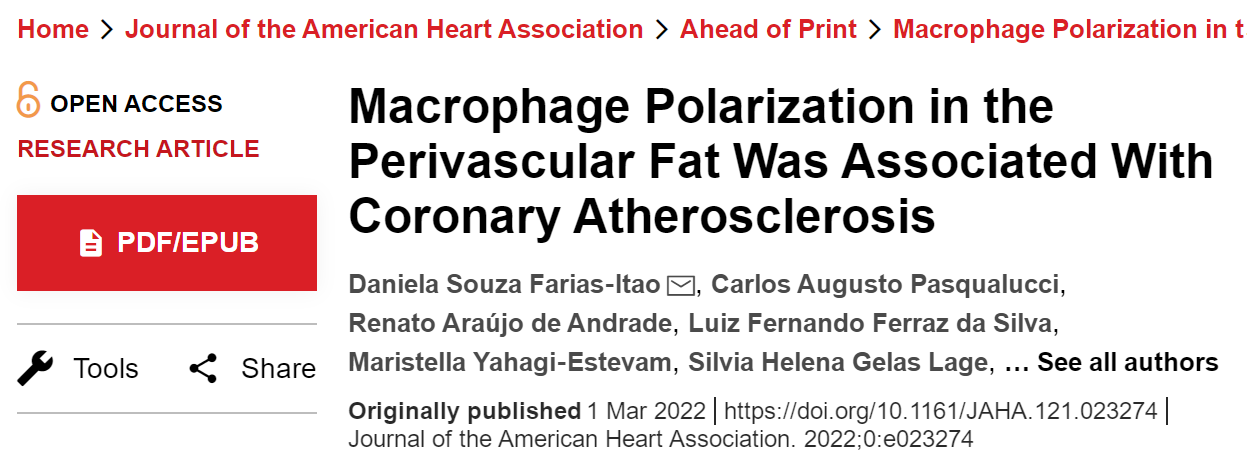
在来自82个受试者的319个冠状动脉节段中,研究人员发现M1/M2巨噬细胞密度比与动脉阻塞程度加重(P=0.02)和脂质含量增加(P=0.01)以及平滑肌细胞减少(P=0.02)相关。M1和M1/M2巨噬细胞的比率与血栓形成风险增加相关(P=0.03)。
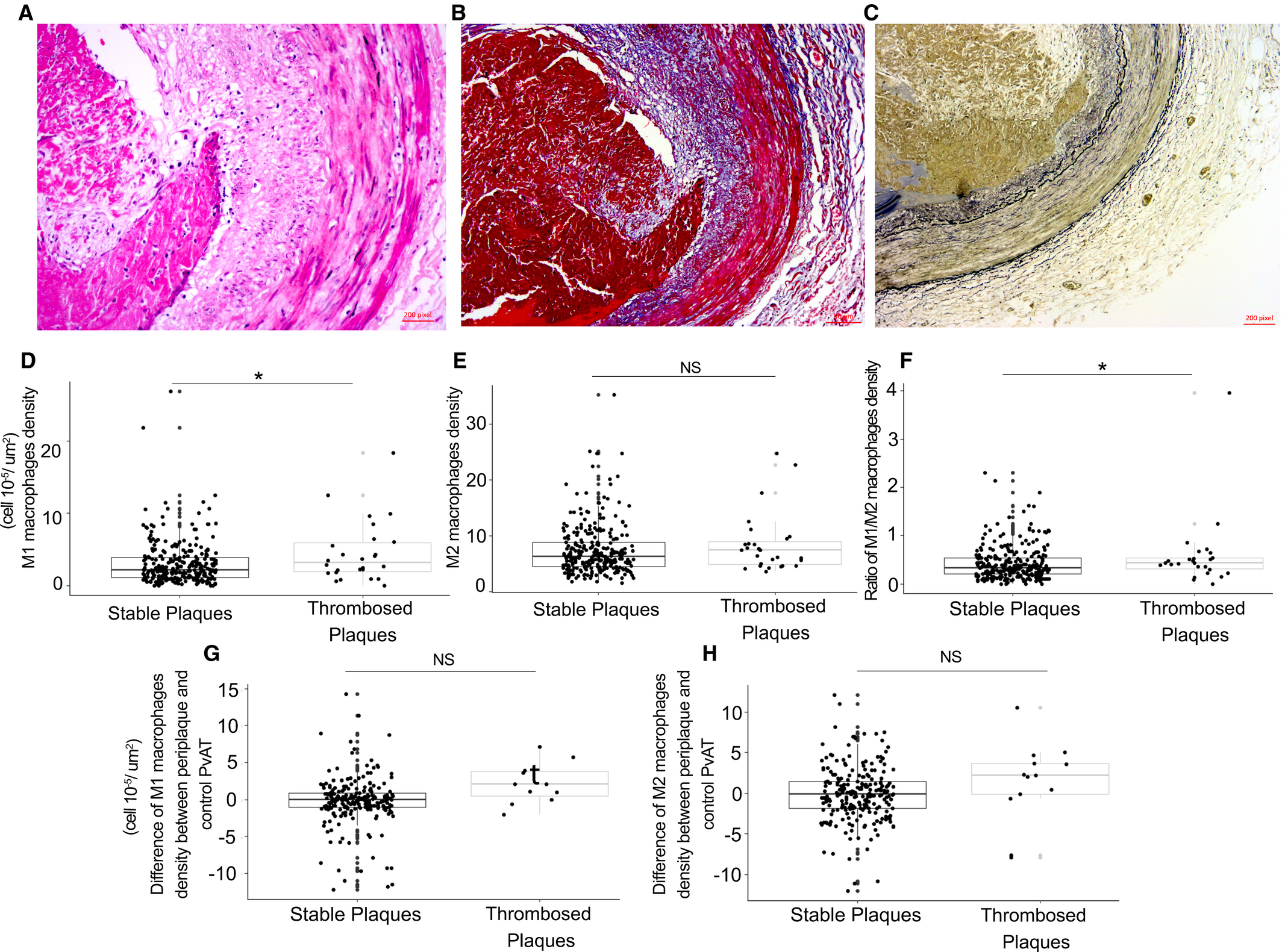
在血栓形成的斑块中,M1巨噬细胞与纤维帽厚度的减少(P=0.006)、脂质含量的增加(P=0.008)和外膜层的滋养血管数量增加(P=0.001)相关。M2巨噬细胞仅在没有血栓形成的斑块中与动脉阻塞程度加重(P=0.01)、钙化(P=0.02)、坏死(P=0.03)相关,而在伴有血栓形成的斑块中血管滋养管数量减少(P=0.003).
由此可见,斑块外周血管周围脂肪组织中的M1巨噬细胞与更高的冠状动脉血栓形成风险相关,并且与斑块进展和不稳定的组织学成分相关。M2巨噬细胞与斑块大小、钙化、坏死含量和外膜层滋养管数量减少相关。
原始出处:
Daniela Souza Farias‐Itao.et al.Macrophage Polarization in the Perivascular Fat Was Associated With Coronary Atherosclerosis.JAHA.2022.https://www.ahajournals.org/doi/full/10.1161/JAHA.121.023274
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#粥样硬化#
53
#冠状动脉粥样硬化#
61
#AHA#
34
#细胞极化#
40