JACC:冠脉CT血管造影是否可替代侵入性冠脉造影?
2021-03-01 MedSci原创 MedSci原创
冠状动脉CTA与ICA评估NSTEACS患者的长期风险的效用相同
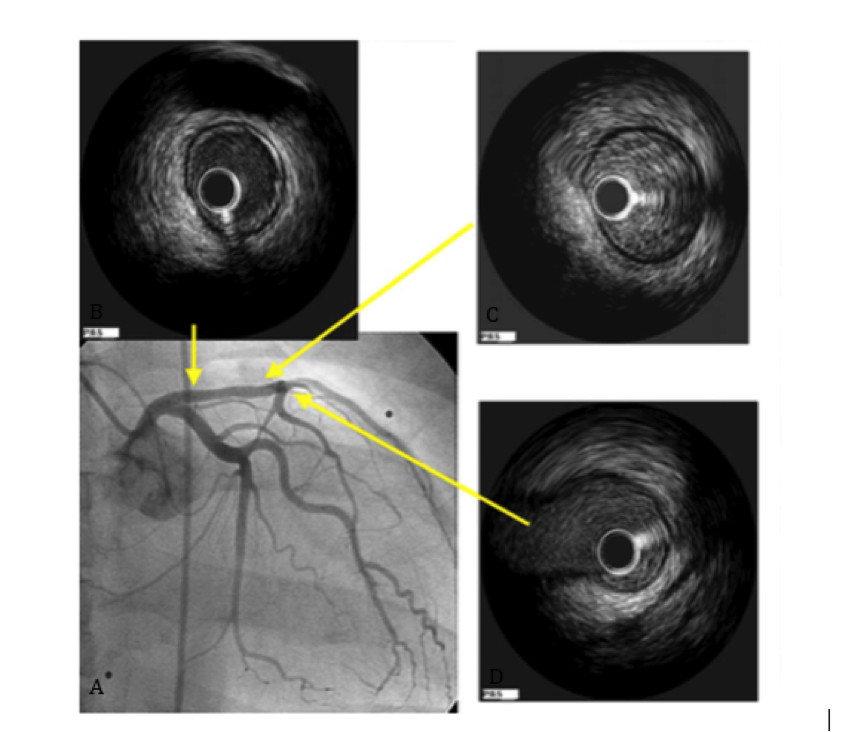
非ST段抬高型急性冠脉综合征(NSTEACS)患者通过侵入性冠状动脉造影(ICA)评估冠状动脉病变(CAD)的严重程度和范围,可指导治疗,并可预测患者的临床预后。
本研究验证了冠状动脉CT血管造影(CTA)与ICA对NSTEACS患者进行风险评估的效用相同的假设。
VERDICT试验评估了NSTEACS患者的治疗时机与临床预后的关系,其中包括在ICA前进行的临床盲法的冠状动脉CTA。CAD的严重程度定义为梗阻性(冠脉狭窄≥50%)或非梗阻性。CAD程度定义为高危(阻塞性左主干或近端左前降支狭窄和/或多支血管疾病)或非高危。主要终点包括全因死亡、非致命性复发性心肌梗死、顽固性心肌缺血住院或心力衰竭。
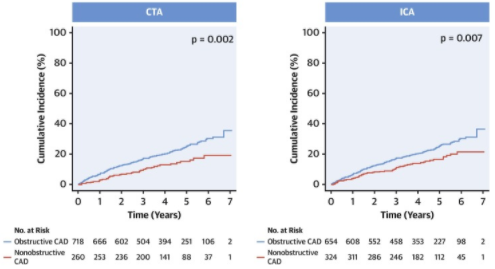
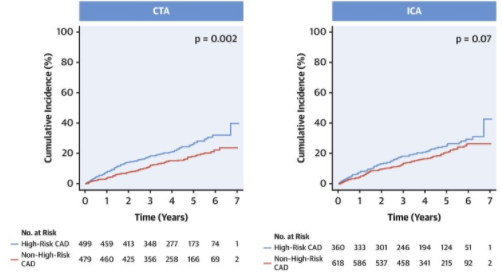
共有978例患者进行了冠状动脉CTA和ICA检查。在中位随访 4.2年(四分位数范围:2.7-5.5年)期间,208名(21.3%)患者出现了主要终点。与冠状动脉CTA(危险比:1.74;95%CI:1.2~2.49;P=0.002)或ICA(1.5;1.13~2.11;P=0.007)定义的非梗阻性CAD患者相比,梗阻性CAD患者的主要终点发生率高1.7倍。
高危CAD患者的主要终点的发生率是冠脉CTA定义的非高危CAD患者的1.5倍(1.56;1.18~2.0 7;P=0.0.002)。ICA也有类似的趋势(1.28;0.98~1.69;P=0.0.07)。
综上,冠状动脉CTA与ICA评估NSTEACS患者的长期风险的效用相同。
原始出处:
Kofoed Klaus F,Engstrm Thomas,Sigvardsen Per E et al. Prognostic Value of Coronary CT Angiography in Patients With Non-ST-Segment Elevation Acute Coronary Syndromes. J Am Coll Cardiol, 2021, 77: 1044-1052.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











学习了
31
#JACC#
30
#侵入性#
50
学习
54
对啊,而且相对的,造影剂使用剂量还少
49
#ACC#
18
#冠脉造影#
41
#造影#
24
#冠脉CT#
25
对于NSTEACS患者CCTA和ICA检查相当的效果
60