Eur Spine J:后外侧经椎弓根入路可完成高危患者脊柱肿瘤切除及360度融合术
2012-08-13 diggs 丁香园
脊柱肿瘤和病理性骨折后的脊髓受压和不稳是疼痛、神经功能障碍及长期制动的原因。除放疗等措施外,脊柱肿瘤也常需手术治疗。脊柱的转移性肿瘤约70%涉及椎体,脊髓受压的部位多在前部或双侧外前部,骨折导致的压迫和不稳经常需前路手术解决。通常,还要结合后外侧减压及后路融合固定术。因此,需要同时面对前-后路手术所致的围手术期并发症,尤其是对于心肺功能异常的基础条件较差的患者
脊柱肿瘤和病理性骨折后的脊髓受压和不稳是疼痛、神经功能障碍及长期制动的原因。除放疗等措施外,脊柱肿瘤也常需手术治疗。脊柱的转移性肿瘤约70%涉及椎体,脊髓受压的部位多在前部或双侧外前部,骨折导致的压迫和不稳经常需前路手术解决。通常,还要结合后外侧减压及后路融合固定术。因此,需要同时面对前-后路手术所致的围手术期并发症,尤其是对于心肺功能异常的基础条件较差的患者,更是使风险倍增。为了改善此类患者的神经功能、提高其生活质量、减轻疼痛,应尝试通过创伤相对小的术式完成减压及脊柱融合。
近期的Eur Spine J杂志上,Sven O. Eicker等德国杜塞尔多夫大学的研究人员发表了其尝试通过单纯后侧入路完成单节段减压及融合固定术的研究。
该研究包括11例转移性脊柱肿瘤、3例脊柱结核或骨质疏松性骨折的患者,均通过后外侧经椎弓根入路进行减压手术,并完成360度融合。平均随访时间7个月,评估指标包括术前术后的VAS(Visual Analog Scale)评分和Frankel评级。
所有患者均于全麻、俯卧位下接受手术,充分暴露后首先以钉棒系统完成固定,通常包括病损部位的上、下各两节椎体,先在肿瘤侵袭较少一侧置棒,然后通过椎板、关节突关节、椎弓根切除来完成减压。在1例胸椎病变的患者,还进行了部分肋-椎横突部分切除术。随后清理侵袭硬膜、神经根的肿瘤,去除被侵袭的骨,切除硬膜前的肿瘤、被侵袭的后纵韧带以获得充分减压。在已经置入的棒的支撑下,可以更好的进行减压,此阶段出血较多,但一旦肿瘤切除完成,则出血量会显着减少,必要时可考虑术前行栓塞术控制术中出血。下一步,经后外侧入路置入一至两枚椎间融合器,融合器中填充自体或异体骨(图 1b,4b)。在行胸椎手术时,可能需牺牲一处神经根,而腰椎则通常不需要。融合器的位置通过术中透视确定,然后置入第二根棒和水平连杆。
图1 后外侧入路经椎弓根360度融合示意图。a 椎体肿瘤侵袭椎弓根和硬膜b 钛质融合器置于切除肿瘤后的缺损区域,并以钉棒系统行后路节段融合术
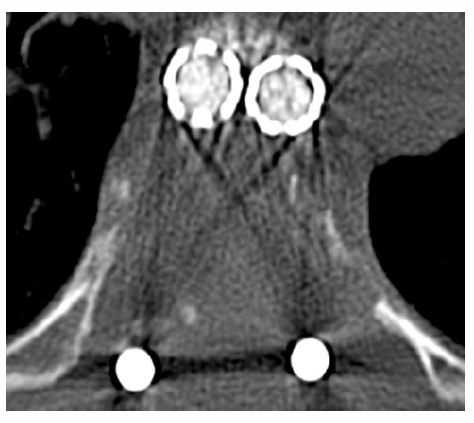
图2 轴位CT显示对胸椎椎弓根狭小的患者通过前路置入融合器完成重建
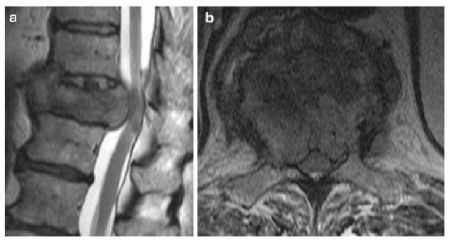
图3 第4例患者初始MRI a 矢状面MRI显示椎体被侵袭、硬膜囊受压迫(胸11)b 轴位MRI显示双侧椎弓根被侵袭。
所有患者的相关情况均在表1中列出,平均手术时间为189.3 ±31.7分钟,2例患者分别在术后1、3个月时因原发肿瘤去世,2例患者在分别随访4、5个月后失访。术中平均失血量为1,096.4 ± 319.5ml,尽管后凸畸形的矫正效果并不明显,但VAS、Frankel评分均获得了显着改善。
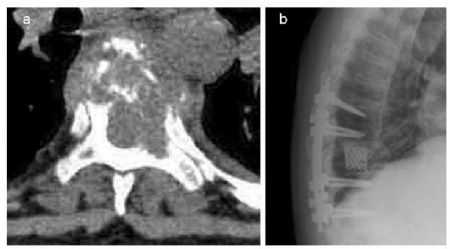
图4a初始轴位CT显示原可作为理想入路的椎弓根被侵袭 b 侧位X线片显示置入融合器完成前柱的重建。
该研究表明,后外侧入路经椎弓根融合固定术可以用于合并心肺系统疾病的患者。后路手术常见的并发症为切口感染(10-62%),此研究中,虽有21%患者出现了切口裂开,但并未出现感染,仅1例患者原有心肺系统疾患加重。因此,作者认为,其所建议的术式可以通过相对小的创伤来完成充分的减压和融合,可改善患者的神经功能、提高生活质量,因其创伤较小,可用于合并心肺系统疾患的脊柱肿瘤患者。但在该文的最后,作者们也指出了该术式的几点不足:1、腹侧病灶的显露可能不充分;2、脊柱肿瘤并不常侵袭后柱结构,如果行椎弓根入路,可能为肿瘤开启了新的侵袭途径,因此,目前此术式一般用于已有相关结构侵袭的患者;3、此入路可能不能有效处理脊柱前的病灶;4、此术式的远期效果尚待长期随访观察。
原文链接:
Eicker SO Cornelius JF Steiger HJ Hänggi D. 360-degree osteosynthesis via a posterolateral transpedicular approach in high-risk patients. Eur Spine J 2012 21 6 :1207-13.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#高危患者#
28
#肿瘤切除#
34
#Spine#
27
#融合#
0
#融合术#
39