瑞芬太尼与心脏手术围术期血糖反应:非盲随机试验
2020-08-12 翻译:佟睿 编辑:冯玉蓉 审校:曹莹 罂粟花
本研究旨在探讨术中输注瑞芬太尼与间断注射芬太尼相比能否减轻择期心脏手术患者术中高血糖和胰岛素抵抗。
背景:本研究旨在探讨术中输注瑞芬太尼与间断注射芬太尼相比能否减轻择期心脏手术患者术中高血糖和胰岛素抵抗。
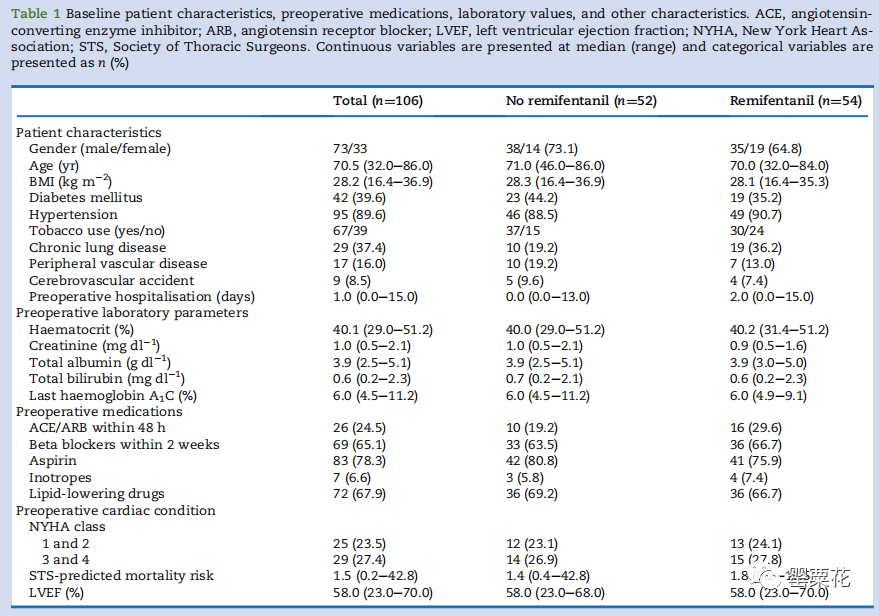
方法:本试验为随机性、前瞻性非盲试验。将择期行心脏手术的患者(n=116)随机分为两组:持续静脉输注瑞芬太尼组和间断注射芬太尼组。从麻醉诱导开始监测24小时内患者每小时的血糖值。主要观察指标为两组之间术中血糖值浓度超过10 mM(180mg .dl-1)的次数≥2次的患者百分比差异。次要结果包括胰岛素需求、选择性应激激素和炎症细胞因子浓度、安全事件和不良后果。
结果:本试验最终纳入了106名受试者进行治疗意向性分析。与芬太尼组(33 [63.5%])相比,瑞芬太尼组术中血糖值两次及以上>10 mM(180mg·dl-1)的患者更少(17 [31.5%])(相对危险度 0.50;95% CI 0.32-0.77;P=0.001)。芬太尼组术中注射胰岛素的中位数为8.1个单位(区间:0-46.7),而瑞芬太尼组为2.9单位(区间:0-35.1)(中位数差异为5个单位;95% CI 1-7;P=0.004)。瑞芬太尼组皮质醇及促肾上腺皮质激素增加减少(P<0.001),但其选择性炎症因子并没有相对减少。两组间术后血糖控制措施和不良临床后果无显著差异。
结论:与间断注射芬太尼的患者相比,持续输注瑞芬太尼的患者在心脏手术期间高血糖的发生率更低,所需胰岛素的用量也更少。
原始文献来源:Subramaniam K, Sciortino C, Ruppert K, et al. Remifentanil and perioperative glycaemic response in cardiac surgery: an open-label randomised trial.[J].Br J Anaesth 2020 Jun ,124 (6): 684-692.
Remifentanil and perioperative glycaemic response in cardiac
surgery: an open-label randomised trial
Abstract
Background: This study investigated whether remifentanil infusion decreased intraoperative hyperglycaemia and insulin resistance compared with intermittent fentanyl administration in patients undergoing elective cardiac surgery.
Methods: This was a randomised, prospective, open-label trial. Patients undergoing elective cardiac surgery (n=116) were randomised to receive either continuous intravenous remifentanil infusion or intermittent fentanyl boluses. Hourly blood glucose values were obtained for 24 h starting from induction of anaesthesia. The difference in percentage of patients with ≥2 intraoperative blood glucose concentrations >10 mM (180 mg dl-1) between the groups was the primary outcome measure. Secondary outcome measures included insulin requirements, select stress hormone and inflammatory cytokine concentrations, and safety events and adverse outcomes.
Results: The trial included 106 subjects in the final intention-to-treat analysis. There were fewer patients with ≥2 intraoperative blood glucose values >10 mM (180 mg dl?1) in the remifentanil group (17 [31.5%]) compared with the fentanyl group (33 [63.5%]) (relative risk: 0.50; 95% confidence interval [CI]: 0.32—0.77; P=0.001). The administered intraoperative insulin was a median of 8.1 units (range: 0-46.7) in the fentanyl group and 2.9 units (range: 0-35.1) in the remifentanil group (median difference=5 units; 95% CI: 1-7; P=0.004). Cortisol and adrenocorticotropic hormone were increased less in the remifentanil group (P<0.001), but there was no relative decrease in this group in select inflammatory cytokines. Postoperative measures of glycaemic control and adverse clinical outcomes were not significantly different between groups.
Conclusions: Compared with patients treated with intermittent fentanyl, patients receiving continuous remifentanil infusion had fewer episodes of hyperglycaemia and less need for insulin administration during the intraoperative period of cardiac surgery.

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#围术期#
53
#芬太尼#
50
#瑞芬太尼#
41
#随机试验#
35
高质量研究,读起来真爽,谢谢梅斯
48