J Child Psychol Psychiatry:自闭症青年感觉反应性的生理与神经指标相关
2021-03-09 MedSci原创 MedSci原创
自闭症谱系障碍青少年表现出对轻度厌恶感觉刺激的高度生理唤醒,尤其是HR反应与SOR的脑和行为有关。
自闭症谱系障碍(ASD)患者通常表现为感觉过度反应(SOR),这是一种与大脑过度反应和对厌恶刺激的行为反应有关的损害状态。虽然ASD患者通常表现出非典型的高度生理唤醒,但这与感觉反应性之间的关系尚不清楚。因此,加利福尼亚大学Jiwon Jung等调查了生理唤醒与SOR的脑和行为指标之间的关系,以帮助理解SOR的生物学机制,并确定生理指标是否与SOR相关的大脑反应有关,研究结果发表在Journal of Child Psychology and Psychiatry杂志。
8~18岁青年(49例ASD,30例年龄、IQ相匹配的典型发育期(TD)经历轻度厌恶触觉、听觉刺激后先行功能磁共振成像(41例ASD,26例TD),然后行皮肤电导(SCR)( 48例ASD,28例TD)和心率(HR)测定(48例ASD,30例TD)。父母报告了他们孩子的SOR严重程度。
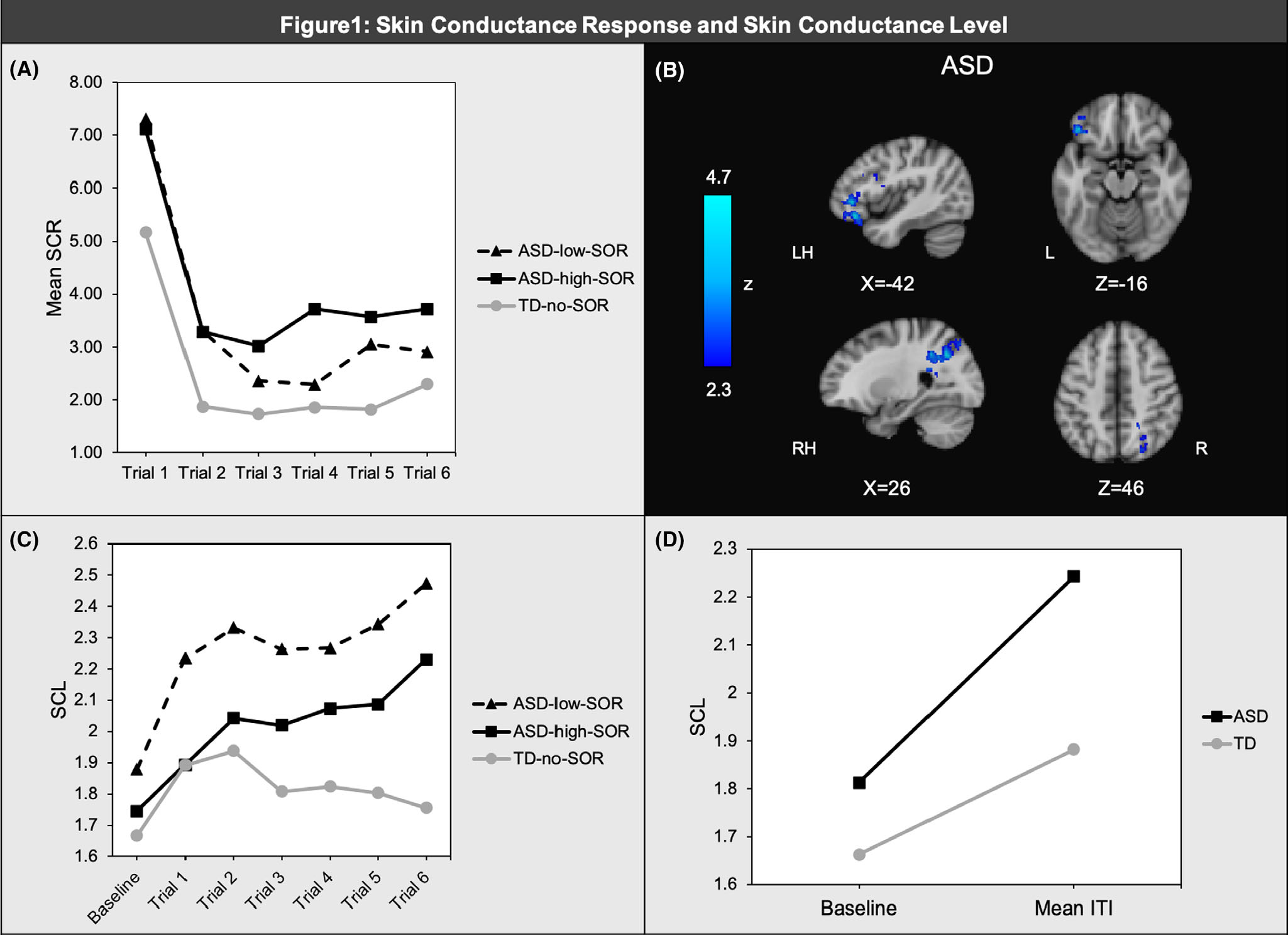
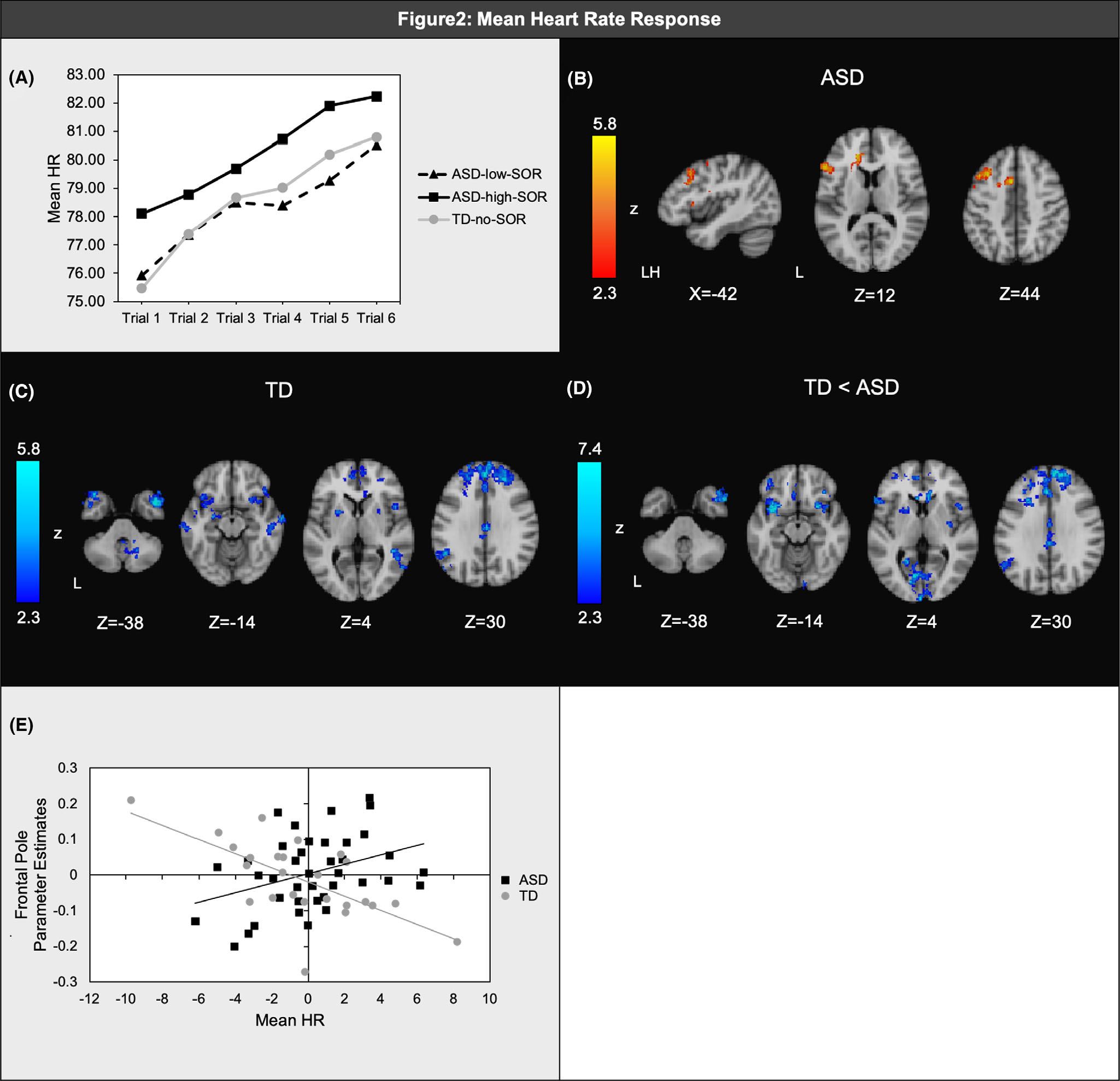
自闭症谱系障碍青年总体上表现出比TD青年更高的SCR和更高的基线心率。以基线心率为协变量,在所有刺激中,ASD中较高的SOR与较高的平均心率相关。此外,与TD组相比,ASD组(尤其是ASD高SOR组)表现出对感觉刺激的HR减速减少/加速增加。在先前与SOR和感觉调节相关的区域,SCR和HR都与大脑对感觉刺激的反应有关。
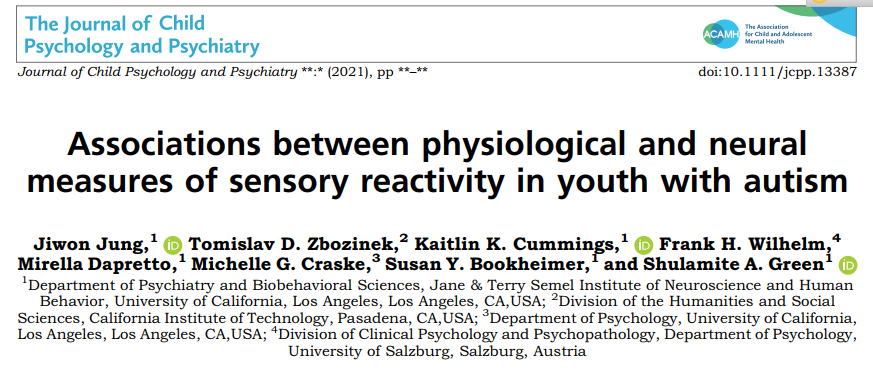
(A)皮肤电导反应(SCR)在联合、触觉和听觉试验中的平均值;(B)ASD内大脑对厌恶感觉刺激的反应与SCR负相关的区域;(C)联合试验前、试验间的皮肤电导水平(SCL);(D)从2分钟基线到所有试验的平均试验间的SCL变化
(A)联合、触觉和听觉试验的平均心率(HR)反应;(B)ASD内大脑对厌恶感觉刺激的反应与平均HR呈正相关的区域;(C)TD内大脑反应与平均HR呈正相关的区域;(D)诊断组间HR和脑反应之间的显著差异;(E)散点图显示各组的平均HR和脑反应之间具有代表性的相关性。
(A)从刺激开始前的5秒到刺激开始后的每个时间点(在水平轴上显示)在关节、听觉和触觉试验中的平均心跳间隔(|B|)变化。前5个时间点(定向和加速阶段)显示1s内的平均|B|,后2个时间点(持续反应/习惯化)显示5s内的平均|B|;ASD(B)和TD(C)内的|B|定向斜率(刺激开始后0-1到1-2s)与大脑对厌恶感觉刺激的反应呈显著负相关;(D) 相对于TD,ASD的定向斜率与脑反应呈较大的负相关;(E)散点图说明各组定向斜率和大脑反应之间的典型相关性。
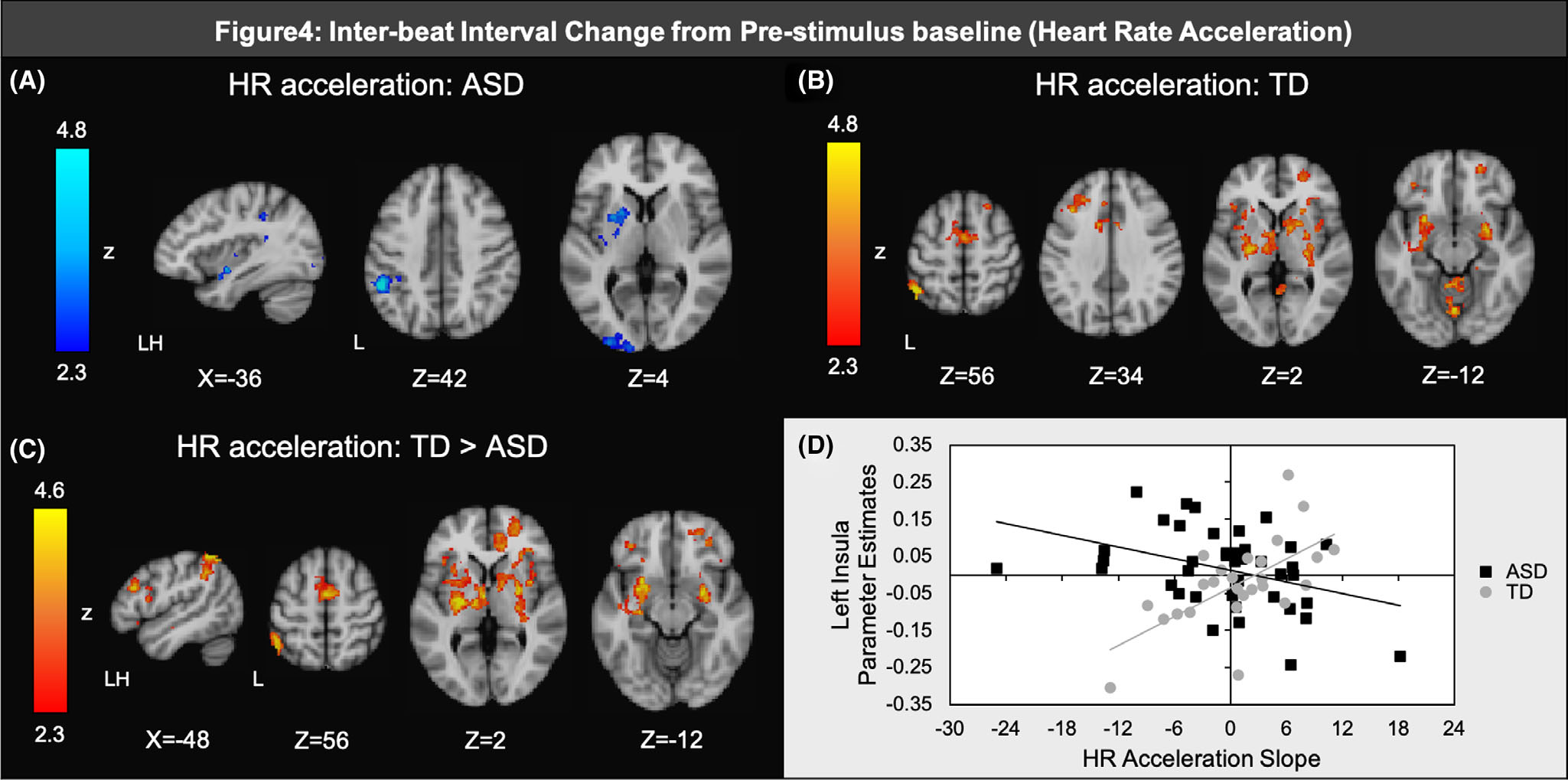
(A)ASD心跳间隔(|B|)频率加速斜率(刺激开始后1 ~ 3 ~ 4 s)与厌恶感刺激脑反应显著负相关(B)TD加速斜率与脑反应显著正相关;(C) 与ASD相比,TD显示与加速度斜率更显著的正相关关系;(D)散点图说明了每组加速斜率和大脑反应之间的典型相关性。
自闭症谱系障碍青少年表现出对轻度厌恶感觉刺激的高度生理唤醒,尤其是HR反应与SOR的脑和行为有关。
综上所述,这些发现表明,心理生理学指标与SOR的行为和神经测量有关,这对于将SOR潜在生物学机制的研究推广到那些可以参与MRI的人群具有重要意义。这些结果对使用心理生理学方法评估SOR有一定的意义,特别是对于不能接受MRI检查的ASD患者。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#反应性#
49
#child#
35
#ILD#
42
#Psychiatry#
55
#自闭#
35
关注
83
真有用
85
自闭症谱系障碍(ASD)患者通常表现为感觉过度反应(SOR)。
92