胸痛患者该做冠脉CT,还是运动试验?JAMA子刊研究
2020-06-09 xujing 文韬 中国循环杂志
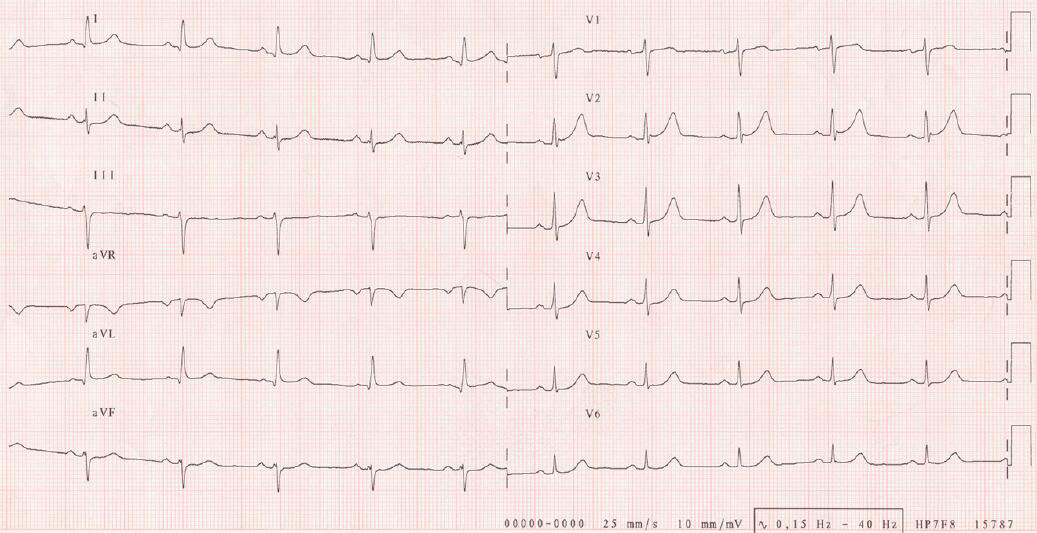
对于疑似冠心病的胸痛患者,心电图运动试验是传统检查手段,诊断冠状动脉狭窄的特异性为85%~90%,但目前冠脉CT应用越来越多,二者有何区别?
对于疑似冠心病的胸痛患者,心电图运动试验是传统检查手段,诊断冠状动脉狭窄的特异性为85%~90%,但目前冠脉CT应用越来越多,二者有何区别?
近期,JAMA心脏病学子刊一项研究发现,在运动试验结果正常或不确定的患者中,存在着大量的非梗阻性和有明显狭窄的冠状动脉疾病。
与随后进行有创冠脉造影对照,运动试验诊断冠心病的特异性达91%,但敏感性仅39%。
对于运动试验异常的患者,5年冠心病死亡或非致命性心梗死亡率增加了2.57倍。
但与运动试验相比,冠脉CT可发现更多冠脉病变。而且其与5年冠状动脉事件的相关性更强。
冠脉CT异常者,5年冠心病死亡或非致死性心梗风险增加了10倍。
作者表示,通过冠脉CT,不但使诊断更为明确,还可以更好的采取预防措施,避免发生严重的心血管事件。
研究发现,对于运动试验结果不确定者,冠脉CT的价值更大。
之前该研究组在新英格兰医学杂志发表的该研究证实,对于胸痛的患者,先做冠脉CT可以明显降低胸痛患者的冠心病死亡及心肌梗死风险,同时不增加介入治疗。
该研究分析了3283例接受运动试验和冠脉CT的患者。
冠脉CT中血管明显狭窄的定义使心外膜大血管管腔横截面积狭窄大于70%,或左主干管腔横截面积狭窄大于50%。冠脉正常为<10%,非梗阻为狭窄10%~70%。
来源:
[1]Singh T, Bing R, Dweck MR, et al. Exercise Electrocardiography and Computed Tomography Coronary Angiography for Patients With Suspected Stable Angina Pectoris: A Post Hoc Analysis of the Randomized SCOT-HEART Trial. JAMA Cardiol. 2020.
[2] Coronary CT Angiography and 5-Year Risk of Myocardial Infarction. The SCOT-HEART Investigators. N Engl J Med, 2018, 379: 924-933.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










值得学习
67
#运动试验#
39
#冠脉CT#
50
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
64