Clin Infect Dis:新的评分办法可预测血液肿瘤患者VRE BSI感染风险
2017-07-20 梁舒瑶 贾朝娟 环球医学
对于血液肿瘤患者,何时使用经验性抗耐万古霉素肠球菌(VRE)抗生素治疗仍是一个临床挑战。2017年6月,发表在《Clin Infect Dis》的一项研究显示,整合VRE定植状态和出现BSI的风险因素是指导血液肿瘤患者合理使用经验性抗VRE微生物疗法的一个有前途的方法。 背景:由耐万古霉素肠球菌(VRE)引起的血液感染(BSI)是血液肿瘤患者的一种重要的并发症。在这一人群中确定何时使用经验性抗V
对于血液肿瘤患者,何时使用经验性抗耐万古霉素肠球菌(VRE)抗生素治疗仍是一个临床挑战。2017年6月,发表在《Clin Infect Dis》的一项研究显示,整合VRE定植状态和出现BSI的风险因素是指导血液肿瘤患者合理使用经验性抗VRE微生物疗法的一个有前途的方法。
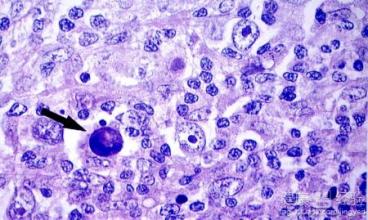
背景:由耐万古霉素肠球菌(VRE)引起的血液感染(BSI)是血液肿瘤患者的一种重要的并发症。在这一人群中确定何时使用经验性抗VRE抗生素治疗仍是一个临床挑战。
方法:一个单中心队列被筛选,包括664名在2006~2014年间因诱导或造血干细胞移植(HSCT)而住院的患者。研究者使用VRE BSI风险因素推导出一个预测评分,并通过计算16232个BSI高风险住院患者日中每日的预测得分,以评估模型的预测性能。
结果:VRE BSI发生率是6.5%(每1000个BSI风险日中有2.7例VRE BSI)。BSI VRE患者的校正1年死亡率和住院时长明显较高。VRE定植(校正比值比[aOR]=8.4;95%置信区间[CI]=3.4~20.6;P<0.0001)、肾功能不全(aOR=2.4;95%CI=1.0~5.8;P=0.046)、氨基糖苷类使用(aOR=4.7;95%CI=2.2~9.8;P<0.0001)与大多数VRE BSI紧密相关,抗厌氧菌抗生素使用(aOR=2.8;95%CI=1.3~5.8;P=0.007)与VRE BSI的相关性最为密切。一个性能最佳的预测模型包括这些因素联合胃肠道紊乱、严重中性粒细胞减少症和先前β-内酰胺抗生素使用。这个评分能有效用于按风险分层的患者(接受者操作特征曲线下面积=0.84;95%CI=0.79~0.89)。在阈值≥5点时,每日VRE BSI概率会增加近4倍。
结论:基于风险因素的新预测评分系统能反映一个似乎合理的血液肿瘤患者VRE BSI病理生理模型。整合VRE定植状态和出现BSI的风险因素是指导血液肿瘤患者合理使用经验性抗VRE微生物疗法的一个有前途的方法。需要验证这个新预测评分,以证实临床效用。
原始出处:
Webb BJ, Healy R, et al. Prediction of Bloodstream Infection Due to Vancomycin-Resistant Enterococcus in Patients Undergoing Leukemia Induction or Hematopoietic Stem-Cell Transplantation. Clin Infect Dis. 2017 Jun 15;64(12):1753-1759. doi: 10.1093/cid/cix232.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Dis#
16
#肿瘤患者#
19
#VRE#
28
学习了受益匪浅。
34
签到学习了很多人
35