新加坡卫生科学局批准继续进行ARCT-021(LUNAR-COV19)疫苗的II期临床研究
2020-12-29 Allan MedSci原创
领先的临床阶段信使RNA药品公司Arcturus Therapeutics今天宣布,该公司已获得新加坡卫生科学局的批准,可以对其候选疫苗ARCT-021进行II期临床研究。
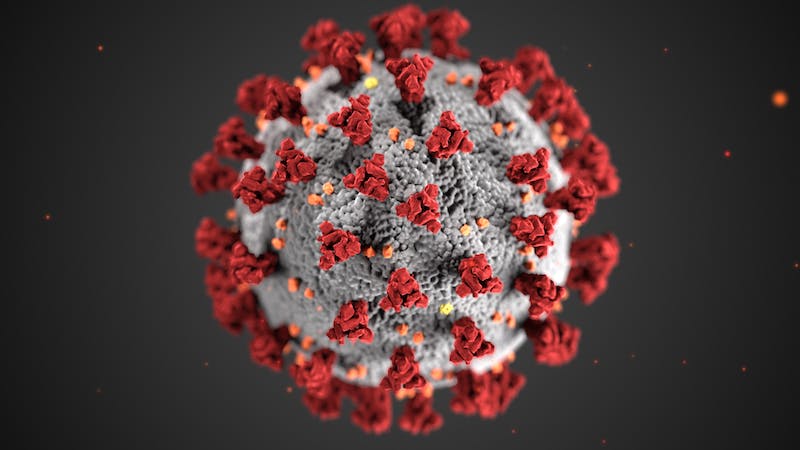
领先的临床阶段信使RNA药品公司Arcturus Therapeutics今天宣布,该公司已获得新加坡卫生科学局的批准,可以对其COVID-19候选疫苗ARCT-021进行II期临床研究。这项研究将基于I/II期临床试验的良好结果以及支持性的临床前数据。

ARCT-021(LUNAR-COV19)的I/II期临床数据显示出良好的耐受性。在100%(44/44)的患者中观察到免疫原性。在灵长类动物攻击模型中,ARCT-021(LUNAR-COV19)在单剂量和初免-再次免疫方案下均显示出保护作用。在耗尽B细胞的体液免疫缺陷动物中,ARCT-021通过单次低剂量给药即可显示出保护作用,进一步强调了ARCT-021细胞免疫的潜在重要性。II期研究将评估多达600名参与者的单剂量和初升-升压方案。预计2021年初的获得II期临床的中期数据。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#II期临床研究#
41
#I期临床#
36
#II期临床#
0
学习
80
学习学习
87
可以
82
学习学习
86
认真学习了
73