Radiology:局部网络效率介导白质高信号病灶体积对认知功能的不利影响
2021-06-12 MedSci原创 MedSci原创
白质高信号体积、局部网络效率和信息处理速度得分是相互关联的,并且局部网络属性解释了由于白质网络变化而导致的较低的认知表现。
脑小血管疾病的病变,例如具有心脏代谢危险因素的个体中的白质高信号(WMH),会干扰白质的运动轨迹,并最终导致认知能力下降。但是,关于确切的基础拓扑机制尚无共识。
Laura W. M. Vergoossen等检查了WMH和认知功能是否相关联,以及在成年人群中是否通过结构连接性措施介导或解释了此类关联。此外,通过评估特定于管道的WMH量及其与认知功能的特定于白质纤维束的联系,调查白质中潜在的局部异常。该研究结果发表在Radiology杂志。

在基于前瞻性2型糖尿病的人群中进行,于2013年12月至2017年2月进行了结构和弥散张量MRI扫描。采集了WMH总体积和特定纤维束的WMH体积、脑网络指标、认知分数、人口统计学资料、心血管和生活方式特征。多变量线性回归和中介分析用于研究WMH体积,特定纤维束的WMH体积以及脑网络与认知功能的关系。根据年龄,性别,教育程度,糖尿病状况和心血管危险因素对关联进行了调整。
入组情况
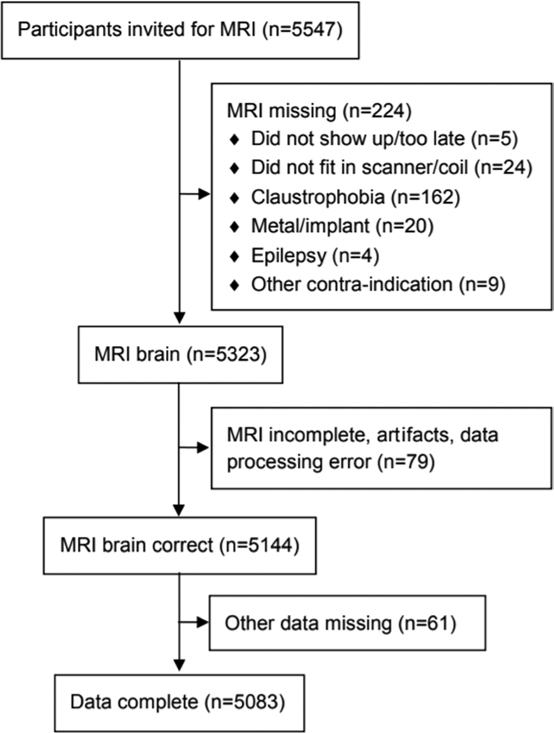
共有5083名参与者(平均年龄,59岁±9 [标准差]; 2592名男性; 1027患有糖尿病)被评估。
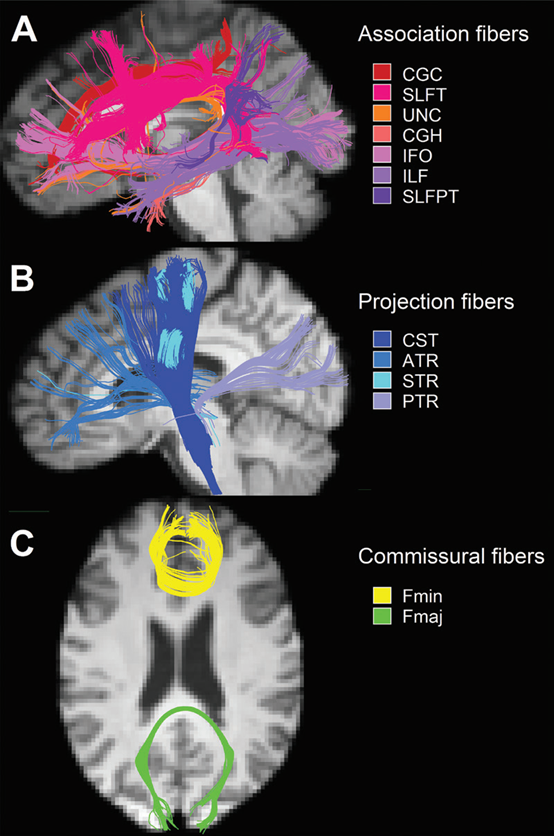
自动图谱引导重建13个预选白质束的三张正交图。A, MRI扫描显示扣带回(CGC)、扣带回海马部分(CGH)、额枕束(IFO)、下纵束(ILF)、上纵束顶部(SLFPT)、上纵束颞部(SLFT)、钩束(UNC)长联合束。B, MRI扫描显示皮质-脊髓束(CST)、丘脑前辐射(ATR)、丘脑后辐射(PTR)和丘脑上辐射(STR)投射束。C, MRI扫描显示大钳(Fmaj)和小钳(Fmin)的连合束。
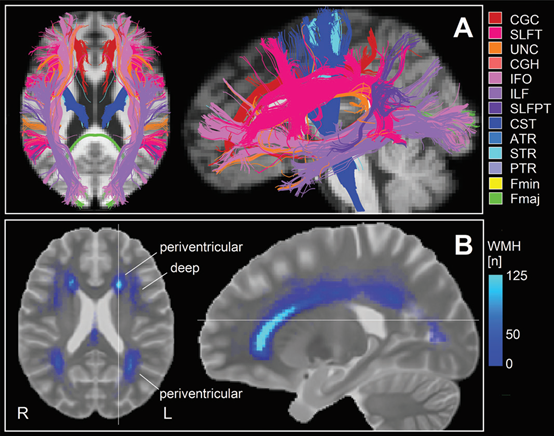
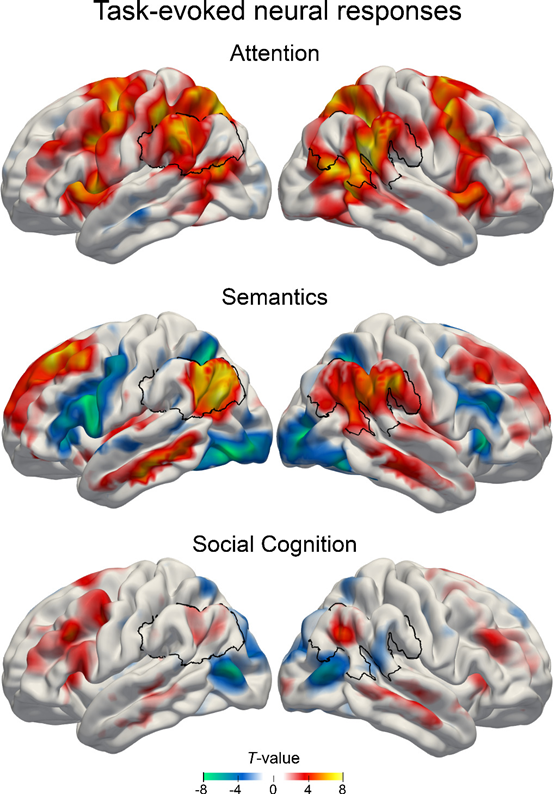
A, MRI扫描显示特定纤维束白质高信号(WMH)体积与信息处理速度得分显著相关(P, 0.05),并根据年龄、性别、教育程度、糖尿病状态和心血管危险因素调整 (模型3)。B,研究样本WMH图。值得注意的是,脑室周围区白质病变的发病率和重叠率较高,而深部病变更普遍。颜色表示在该体素中有WMHs的受试对象数量。
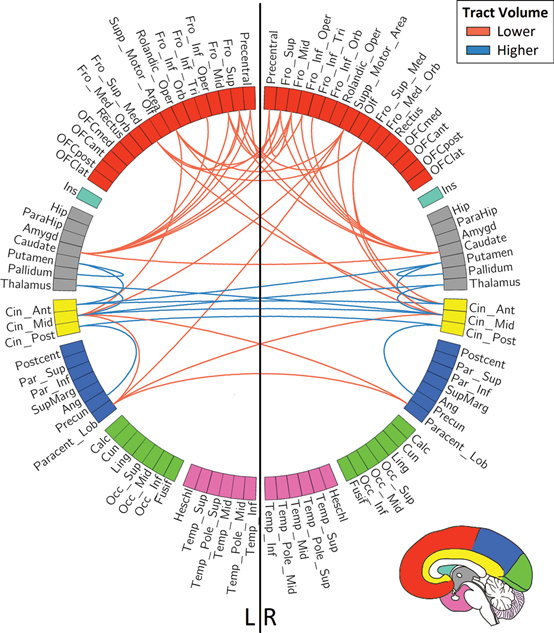
基于Fazekas评分,连接图定性描述了100个自动解剖标记图谱区域之间的白质束,束体积在组间有最大(绝对)差异。红线表示白质高信号组的体积小的纤维束(Fazekas评分≥1 vs 0),蓝线表示体积大的纤维束。

白质高信号(white matter hyperintensity, WMH)体积、局部网络效率和信息处理速度(information processing speed, IPS)得分之间的关系,以及局部效率的中介作用。实线表示直接效应(c9);虚线表示间接影响(a∙b)和百分比介导(百分比介导[PM] = indirect/total = indirect/[indirect + total])。这些关联以标准化回归系数(标准化b)给出,并根据年龄、性别、教育程度、颅内容积、糖尿病状态、MRI补丁更新、体重指数、总胆固醇与高密度脂蛋白的比值、收缩压、脂质修饰和抗高血压药物和先前的心血管疾病进行调整。* = p, 0.01。
更大的WMH体积与更强的局部网络效率 (标准化β系数, 0.065; P < .001)、较低的信息处理速度 (标准化β系数, −0.073; P < .001)相关。此外,较低的局部效率 (标准化β系数,−0.084;P<0.001)与较低的信息处理速度有关。特别是,WMHs与信息处理速度之间的关系通过局部网络效率中介(中介百分比,7.2% [95% CI: 3.5, 10.9];P<0.05)。最后,在对信息处理速度有重要影响的白质束中,WMH负荷较大。
综上所述,该研究发现白质高信号(WMH)病灶体积、局部网络效率和信息处理速度得分是相互关联的。更具体地说,更大的WMH体积对认知功能的不利影响是由局部网络效率介导的。局部研究发现,白质束中对信息处理非常重要的WMH体积越大,认知速度越慢,这反映了具有心脏代谢危险因素的老年个体中,由于白质病理特征导致的认知能力下降。
原文出处
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#白质#
33
#白质高信号病灶#
34
#高信号#
33
#局部#
35
#白质高信号#
44