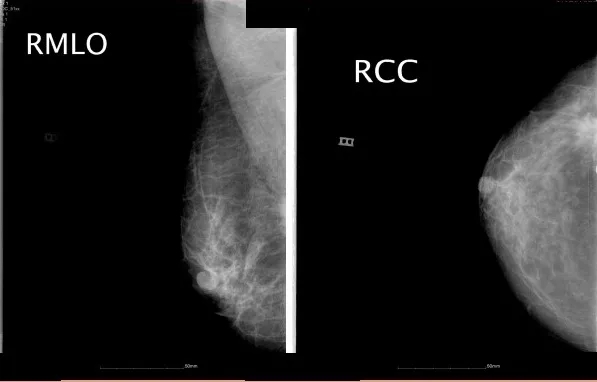
JCO:地塞瑞克与曲普瑞林治疗局部晚期内分泌反应性乳腺癌:随机II期试验
2018-12-30 海北 MedSci原创
最近,研究人员进行了一项临床试验,在接受来曲唑作为乳腺癌新辅助内分泌治疗的绝经前患者中,评估地塞瑞克(一种促性腺激素释放激素[GnRH]拮抗剂)与曲普瑞林(一种GnRH激动剂)的卵巢功能抑制(OFS)对内分泌活性的影响。
最近,研究人员进行了一项临床试验,在接受来曲唑作为乳腺癌新辅助内分泌治疗的绝经前患者中,评估地塞瑞克(一种促性腺激素释放激素[GnRH]拮抗剂)与曲普瑞林(一种GnRH激动剂)的卵巢功能抑制(OFS)对内分泌活性的影响。
该试验招募的标准为:患有乳腺癌的绝经前妇女,分期为cT2至4b,任何N,M0;雌激素受体和孕激素受体大于50%;人类表皮生长因子受体2阴性。受试者在每个周期的第1天肌内注射曲普瑞林3.75 mg,或在第1周期第1天皮下给予地塞瑞克240 mg(SC),然后在第2到第6周期第1天肌肉注射80 mg SC。两组受试者均使用来曲唑2.5毫克/天,持续6个28天的周期。受试者在最后一次注射后2至3周进行手术。
研究人员在基线,24和72小时后,第7天和第14天,然后在第2至第6周期注射之前收集血清。该试验的主要终点是最佳OFS的时间(在新辅助治疗期间,从第一次注射到首次评估的雌二醇水平≤2.72pg/ mL [≤10pmol/ L]的时间)。使用对数秩检验,双侧α为0.05,该试验具有90%的能力来检测差异。
次要终点包括反应,耐受性和患者报告的内分泌症状。
在2014年2月至2017年1月期间,该试验招募了51名患者(n = 26名接受曲普瑞林加来曲唑;n = 25名接受地加瑞克加来曲唑)。分配到地加瑞克和来曲唑的患者的最佳OFS时间比使用曲普瑞林和来曲唑的时间快3倍(中位数,3 v 14天;风险比,3.05;95%CI,1.65至5.65;P <.001)。此外,对于所有接受地加瑞克和来曲唑的患者,在随后的周期中可以维持OFS,而在第1周期(在127次测量期间的6个事件)中,15.4%被指定接受曲普瑞林和来曲唑的患者具有次优的OFS。两者引起的不良事件如预期。
在接受来曲唑用于新辅助内分泌治疗的绝经前妇女中,相比使用曲普瑞林,使用地加瑞克可以更有效地实现OFS,并且可以更有效地维持OFS。
原始出处:
Dellapasqua S et al. Neoadjuvant Degarelix Versus Triptorelin in Premenopausal Patients Who Receive Letrozole for Locally Advanced Endocrine-Responsive Breast Cancer: A Randomized Phase II Trial. JCO, 2018; doi: 10.1200/JCO.18.00296.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#局部晚期#
26
#II期试验#
20
#分泌#
19
#JCO#
26
#反应性#
30
#曲普瑞林#
34
#局部#
16