心肺联合超声在间质性肺疾病中的临床应用进展
2016-09-07 朱维维 吕秀章 李一丹 首都医科大学附属北京朝阳医院心脏超声科 中华超声影像学杂志
间质性肺疾病(interstitial lung diseases,ILD)是一类较为复杂的疾病,种类繁多,其共同的病理学表现为间质水肿、纤维素渗出、成纤维细胞成簇状增生累及肺泡腔及小叶间隔。目前国内尚未有确切流行病学资料报道ILD的发病率及死亡率,据王柳盛等的调查,近年来ILD在中国大陆的发病率有明显上升趋势,重庆市和天津市统计的住院ILD患者中,住院期间病死率分别为8.68%和10.2%。
间质性肺疾病(interstitial lung diseases,ILD)是一类较为复杂的疾病,种类繁多,其共同的病理学表现为间质水肿、纤维素渗出、成纤维细胞成簇状增生累及肺泡腔及小叶间隔。目前国内尚未有确切流行病学资料报道ILD的发病率及死亡率,据王柳盛等的调查,近年来ILD在中国大陆的发病率有明显上升趋势,重庆市和天津市统计的住院ILD患者中,住院期间病死率分别为8.68%和10.2%。ILD呈渐进性发展,随着肺泡毛细血管膜弥漫性受损,最终可导致肺动脉高压和呼吸衰竭。因此,有效监测ILD患者心肺情况有助于改善疾病预后。目前临床上评价ILD心肺情况的方法主要有肺高分辨率CT(简称肺CT)、肺功能试验(PFTs)及超声心动图。肺CT是临床上无创评估ILD的金标准,因具有放射性、价格昂贵、不能进行床旁检查等缺点,在监测和管理ILD中存在着一定限制。近年来,有学者将肺超声应用于ILD中,发现肺超声能够精确评估ILD肺部情况,是肺CT的重要补充。超声心动图可无创评估肺动脉压力及右心功能,早期发现ILD患者心脏受累。因此,肺超声联合超声心动图(简称心肺联合超声)为临床诊断和管理ILD患者提供了新的方法。
一、间质性肺疾病基本特征
1.分类:
ILD包括200多种急、慢性肺部疾病,根据病因、临床及病理特点,2002年美国胸科协会及欧洲呼吸学会将ILD分为四大类:①已知原因ILD,如结缔组织疾病相关性ILD;②特发性间质性肺炎(IIP),如特发性肺间质纤维化(IPF);③肉芽肿性ILD;④罕见ILD,如肺泡蛋白沉积症(PAP)。我国ILD病种分布以IPF及结缔组织相关性ILD为主。
2.病理生理学改变:
ILD种类繁多,病理学表现各异,其共同的病理进程大致分为4个阶段。最初表现为肺组织实质损伤和肺泡炎,伴实质细胞增生,肺泡间隔细胞成分增加。慢性进展病例最终出现肺泡间隔纤维成分增多,肺泡壁及小叶间隔增厚。肺泡炎性损伤进行性加重致使肺泡壁结构破坏,肺泡融合呈囊状、蜂窝状。这些结构改变导致肺顺应性下降,功能性肺泡细胞减少,肺通气/血流(V/Q)比值下降。肺总量及肺活量下降,呼吸做功量增加,继而患者出现运动耐力下降及呼吸困难。ILD并发肺动脉高压及肺心病者较多。据流行病学调查研究,ILD中IPF患者肺动脉高压的发病率最高,早期阶段8%~11%,进展阶段32%~46%,终末期86%。目前,ILD并发肺动脉高压的发病机制尚不明确,被认为与缺氧性血管收缩、血管活性物质改变(如血管内皮素-1)、肺血管阻力、血管解剖结构的急慢性改变以及遗传变异有关。
二、肺超声在ILD中的应用
1.肺超声简要扫查技术:
肺超声扫查仅需普通超声仪即可。目前,尚未建立一套最佳肺超声扫查方法。ILD肺部超声扫查方法较为简便,运用较为广泛的为Jambrik等推荐的前侧胸壁28点扫查法(图1)。由于ILD特异性病理分布特点,Gargani等建议扫查患者双侧后胸壁(图2)。普通二维心脏探头、凸阵/微小凸阵探头以及线阵探头均可进行肺超声扫查。不同探头观察侧重点不同,低频探头用于观察B线、胸腔积液及深部肺实变,高频探头用于观察胸膜、胸膜滑动情况及引导肺穿刺。扫查时患者体位不受限制,可采取仰卧位或坐位。
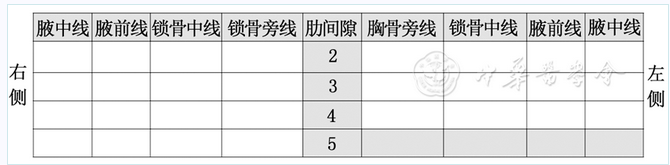
图1双侧前侧胸壁28点扫查法,空白处为扫查区域

图2双侧后胸壁扫查区域,空白处为扫查区域
2.肺超声在ILD中的应用进展:
长久以来,肺部被视为超声扫查的禁区。1997年Lichtenstein等首次描述了肺泡间质综合征与肺"彗星尾征"(B线)的关系,从此开创了肺超声应用于临床的先河。B线的产生源于超声束在增厚小叶间隔或水肿肺泡内来回往返,形成多次反射,声像图上表现为"彗星尾征"。ILD特征性肺超声表现为:①双肺多发分布不均的B线(大多分布于双侧肺底及背侧);②胸膜线异常(不光滑、破碎状),胸膜增厚(>2.8 mm),胸膜滑动减弱;③胸膜下小无回声区;④微量胸腔积液。ILD不同病理发展阶段肺超声表现不同,Sperandeo等针对这一问题分享了一些他们的经验。轻度肺间质纤维化表现为仅分布于两肺底部的B线及不规则增厚胸膜线;中、重度肺间质纤维化表现为多发弥散分布于整个肺表面的B线、破碎状胸膜线及胸膜下小无回声区,严重者可出现胸膜滑动减弱。因此,Sperandeo等认为肺超声是一个诊断和监测ILD的可靠工具。
Gargani等通过比较系统性硬化症(systemic Sclerosis,SSc)患者肺超声、肺CT及肺功能试验结果,提出了一些新的看法,他们发现肺超声不仅能够诊断ILD,而且B线数目与肺CT及肺功能试验评估的疾病严重程度呈正相关,并给予B线高度评价,认为它是一个简单、无辐射、可用于床旁诊断SSc患者潜在肺纤维化及判断预后的重要超声标志。随后,Gutierrez等在此基础上对不同程度间质性肺疾病B线数目进行了半定量评分:0分,正常(<10条);1分,轻度(11~20条);2分,中度(21~50条);3分,重度(>50条)。Tardella等以肺CT为标准对该评分的可靠程度进行了分析,结果显示B线半定量评分与肺CT Warrick评分及反映肺通气功能障碍的DLCO值存在良好相关性,因此认为该评分可以作为结缔组织病所致肺纤维化患者的补充评估方法。Hasan等在一整组间质性肺疾病中验证了此前的研究,并发现了一些新的问题。以往研究表明依据B线的间距可以区分间质肺水肿和肺泡肺水肿,同样,B线的间距也可以用来评估ILD严重程度,而且B线间距≥7 mm常提示肺广泛纤维化及蜂窝肺。
早年应用肺超声评估ILD严重程度的方法均集中于B线的数目及分布。尽管此前关于ILD的描述中提及了胸膜线表现,但目前尚未有确切肺超声综合评估ILD严重程度的方法。近年来,不少学者在这一方面做出了许多贡献。Moazedi-Fuerst等在评估肺超声检出RD患者肺纤维化的诊断价值研究中提出了一套肺超声综合评估方法,但这项研究并没有验证其评估ILD严重程度的可靠性。近期Buda等以肺CT Warrick评分为基础,衍生出了一套肺超声评估结缔组织病肺纤维化严重程度的综合评估方法。该研究中将B线、胸膜线与特定肺CT征象一一对应起来:磨玻璃影—白肺;小叶间间隔增厚—不规则,凹凸不平,碎片状胸膜线;小叶内间隔增厚—B线,不规则胸膜线;蜂窝影—模糊状胸膜线。虽然肺超声在评估ILD严重程度方面仍存在着或多或少的局限性,但联合超声心动图评估其他影响预后的因素,如肺动脉高压、右室功能障碍等,在管理和治疗中也是必不可少的。
三、超声心动图在ILD中的应用进展
毛细血管前肺动脉高压常出现在ILD的进展阶段,与高死亡风险有关。ILD合并肺动脉高压患者的生存率与右心功能密切相关。Rivera-Lebron等通过随访分析135例IPF终末期进行肺移植患者生存情况,指出右心结构和功能变化是影响IPF肺移植患者生存率的关键因素,建议临床上应用超声心动图评价ILD患者右心结构和功能,更好地识别高危人群。然而,早期ILD患者右心结构、功能变化及进展情况仍需进一步探索。最近,D'Andrea等运用传统超声心动图及二维斑点追踪超声心动图(speckle tracking echocardiography,STE)对伴或不伴肺动脉高压IPF患者右心结构和功能展开研究,结果显示无论IPF患者伴或不伴肺动脉高压,右心功能均出现不同程度减低,并且较传统超声心动图而言,STE能够发现无症状IPF患者早期右心功能减低。这是目前较为少见的将STE应用于ILD中的研究。
迄今为止,超声心动图应用于间质性肺疾病中的研究相对较少。ILD以肺实质结构和弥散功能改变为主,间接影响心脏结构及功能,这可能是目前忽视ILD右心结构和功能变化的主要原因。
四、心肺联合超声在间质性肺疾病中的应用
1.优势:
心肺系统是互相关联的,因此心肺联合超声技术的发展也是必然的。肺超声能够发现肺、胸膜、胸腔病变,联合超声心动图评估心脏结构及功能,判断有无心脏受累,为临床管理ILD提供更多信息。虽然心肺联合超声在间质性肺疾病中的应用尚不成熟,但该项技术已广泛应用于急重症疾病当中。Lichtenstein等给予心肺联合超声技术高度评价,认为心肺联合超声是一个强大的诊断和监测工具,可以称之为ICU医生的"眼睛"。国内学者Zheng等将心肺联合超声应用于分析ILD患者B线与肺动脉压力之间的关系,研究表明B线条数与肺动脉收缩压(PASP)呈正相关,且B线>4条提示PASP>30 mmHg。这也是目前为止极少数将心肺联合超声应用于ILD中的研究。心肺联合超声应用于ILD中的优势表现在:①较肺CT而言,心肺联合超声具有经济、无辐射、可进行床旁检查的优点;②心肺联合超声能够发现无症状ILD患者肺部早期改变,建立有效随访;③心肺联合超声能够监测ILD疾病进展,评估右心功能及肺动脉压力,提早发现高危人群,改善预后。
2.不足:
任何一种诊断方式都存在一定的局限性。心肺联合超声应用于ILD中的局限性主要体现在:①对于肥胖、皮下气肿患者,超声束传播受到限制;②肺超声扫查结果定量、定性分析容易受主观因素影响;③肺超声扫查方式及ILD严重程度评估方法,仍然备受争议;④超声心动图能否有效评估ILD患者早期右心功能变化,也是目前值得关注的问题。
五、展望
心肺联合超声作为诊断和监测ILD心肺情况的良好工具,为临床管理疾病提供更多有效信息。目前心肺联合超声应用于ILD的研究较少,主要局限于疾病的某一类型。超声心动图新技术迅猛发展,但应用于ILD中的研究依然较少。因此大规模、前瞻性联合应用超声心动图新技术的研究是必不可少的。心肺联合超声技术尚处在发展阶段,也存在着一定的不足。但随着超声技术的发展以及研究的深入,心肺联合超声在间质性肺疾病中的应用将有着更为广阔的前景。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#心肺#
31
#临床应用#
26
#间质性#
28
#应用进展#
30
很好,不错,以后会多学习
51
很好,不错,以后会多学习
46
很好,不错,以后会多学习
44
肺超声联合心脏超声心动图(心肺联合超声)为临床诊断和管理ild患者提供了新的方法。
46
hrct是无创评估ild的金标准,具有放射性、价格昂贵、不能进行床旁检查。
43
这篇咨询不错哦,值得学习,对于临床工作和科研思路都很有帮助。
26