JCEM:恩格列净的心血管益处与2型糖尿病患者肠道微生物和血浆代谢物相关
2022-04-10 MedSci原创 MedSci原创
恩格列净可能是伴有心血管疾病风险的2型糖尿病患者的首选治疗方案;它的心血管益处可能与肠道微生物群和血浆代谢物的变化有关。
恩格列净对2型糖尿病(T2DM)患者的心血管益处已有报道;然而,潜在的机制仍然是未知的。近日,内分泌和代谢性疾病领域权威杂志Journal of Clinical Endocrinology & Metabolism上发表了一篇研究文章,研究人员假设恩格列净对心血管的益处与肠道微生物群和血浆代谢产物的改变有关,恩格列净可能用于有心血管疾病风险的T2DM患者的初始治疗。
该研究为随机、开放标签的为期3个月的两组临床试验,纳入了76例未治疗的伴有心血管疾病危险因素的T2DM患者。受试者接受恩格列净 (10 mg/d, n=40)或二甲双胍(1700 mg/d, n=36)治疗。
研究人员探究了与葡萄糖代谢和心血管疾病危险因素相关的临床参数的变化,并使用16S rRNA基因测序的肠道微生物群以及使用LC-MS的血浆代谢产物进行了分析。
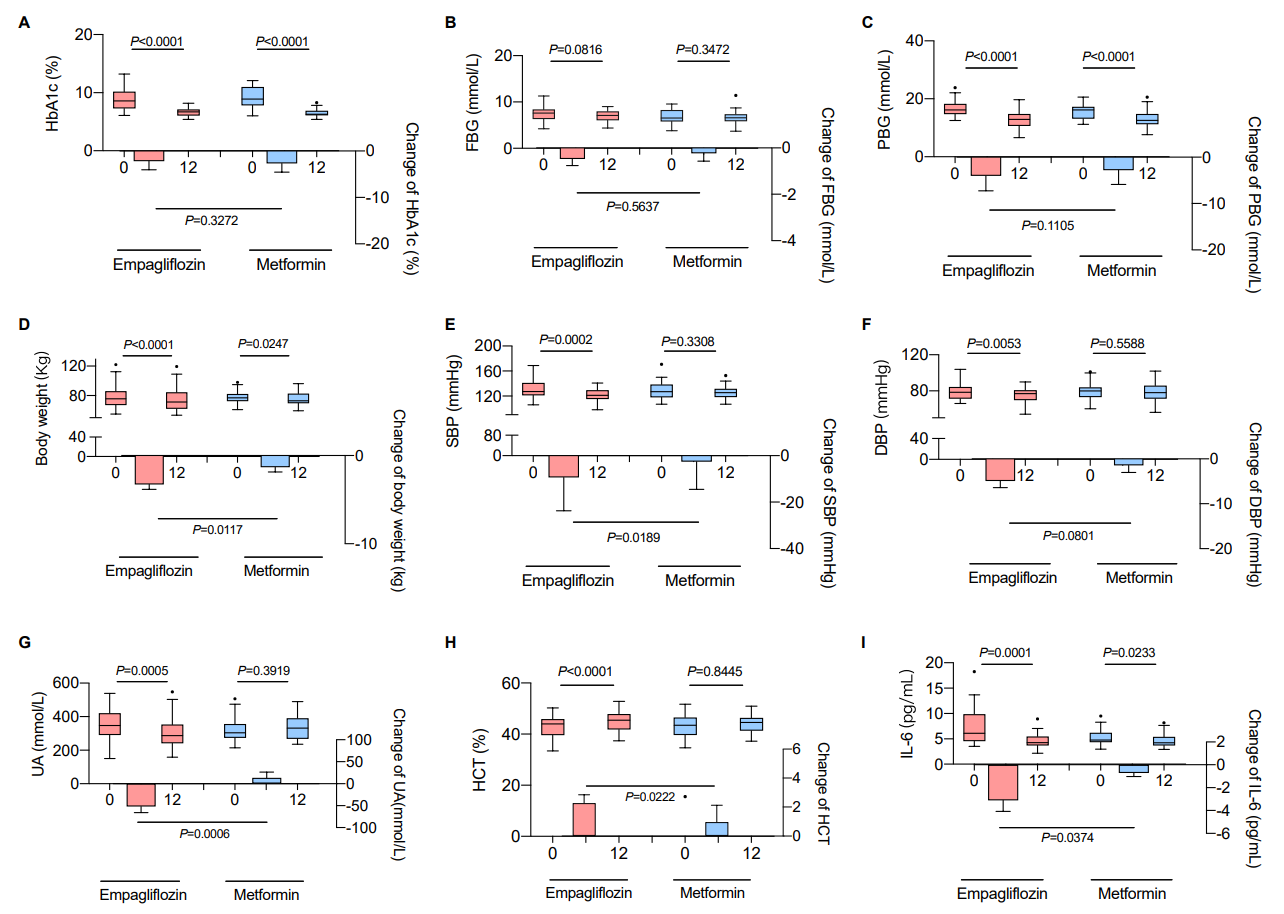
研究人员发现,两组患者的糖化血红蛋白水平均有显著且相似程度地降低,糖代谢也有所缓解。然而,只有恩格列净能改善心血管疾病的危险因素。治疗1个月后,恩格列净显著重塑了肠道菌群;这一变化一直保持到研究结束。恩格列净增加了血浆代谢产物如鞘磷脂的水平,但降低了糖基鹅去氧胆酸、顺式乌头酸和尿酸的水平。同时,恩格列净提高了生产短链脂肪酸细菌的水平,如来自Roseburia、Eubacterium和Faecalibacterium,并减少包括大肠杆菌、志贺氏菌、嗜胆菌和 Hungatella在内有害细菌的水平。
由此可见,恩格列净可能是伴有心血管疾病风险的2型糖尿病患者的首选治疗方案;它的心血管益处可能与肠道微生物群和血浆代谢物的变化有关。
原始出处:
Xinru Deng.et al.Cardiovascular benefits of empagliflozin are associated with gut microbiota and plasma metabolites in type 2 diabetes.JCEM.2022.https://academic.oup.com/jcem/advance-article/doi/10.1210/clinem/dgac210/6565990
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#微生物#
33
#JCE#
33
#代谢物#
34
#JCEM#
29
#血浆代谢物#
34
#2型糖尿病患者#
28
#糖尿病患者#
28
已经学习了
61
学习
59
学习了
50