Frontiers in Oncology:双管齐下:化疗减瘤+CAR-T治疗,提高高肿瘤负荷淋巴瘤患者缓解率和总生存率
2021-08-17 “E药世界”公众号 “E药世界”公众号
近日,南开大学附属第一中心医院邓琦主任医师团队等在 Frontiers in Oncology (IF=6.244)期刊发表了题为:Intensive Debulking Chemotherapy I
难治性/复发性(R/R)弥漫性大 B 细胞淋巴瘤(DLBCL)的治疗反应和预后较差。目前的标准治疗包括大剂量化疗,然后是自体干细胞移植。然而,此类治疗相关的长期缓解率仅为10-20%。
2017年至今,已经有5款CAR-T细胞疗法上市,CAR-T疗法在 B 细胞恶性肿瘤中显示出显着效果。之前的临床试验显示其对 B 细胞淋巴瘤的客观缓解率达50-80%,完全缓解率达30-50%。NCCN指南也推荐CAR-T疗法用于二线治疗后获得部分缓解的弥漫性大 B 细胞淋巴瘤(DLBCL)患者以及二线治疗获得完全缓解后复发或疾病进展的患者。
CAR-T疗法通常与潜在的致命毒性有关,包括细胞因子释放综合征(CRS)和神经系统毒性,尤其是在肿瘤负荷高的情况下。此外,高肿瘤代谢体积已经被明确为CAR-T治疗 弥漫性大 B 细胞淋巴瘤(DLBCL)早期进展的预测因素。因此,在开始CAR-T治疗之前,通过强化化疗降低肿瘤负荷,能够提高CAR-T治疗效果。
近日,南开大学附属第一中心医院邓琦主任医师团队等在 Frontiers in Oncology (IF=6.244)期刊发表了题为:Intensive Debulking Chemotherapy Improves the Short-Term and Long-Term Efficacy of Anti-CD19-CAR-T in Refractory/Relapsed DLBCL With High Tumor Bulk 的临床研究论文。
该团队之前已经证明,难治性/复发性 B 细胞急性淋巴细胞白血病 (B-ALL) 中的CAR-T 疗法与强化淋巴细胞清除化疗后的高治疗反应和可控的毒性有关。
强化化疗常用于难治性/复发性(R/R)弥漫性大 B 细胞淋巴瘤(DLBCL)的治疗方案,例如DHAP(地塞米松、顺铂和阿糖胞苷)、DA-EPOCH(剂量调整的依托泊苷、泼尼松、长春新碱、环磷酰胺和多柔比星)、ICE(异环磷酰胺、卡铂和依托泊苷)和 GemOx(吉西他滨和奥沙利铂)。
由于许多肿瘤体积较大的难治性/复发性(R/R)弥漫性大 B 细胞淋巴瘤(DLBCL)患者在强化化疗后肿瘤负荷能够暂时降低,因此,研究团队猜测减少患者的肿瘤负荷能够提高抗CD19-CAR-T细胞治疗的效果。
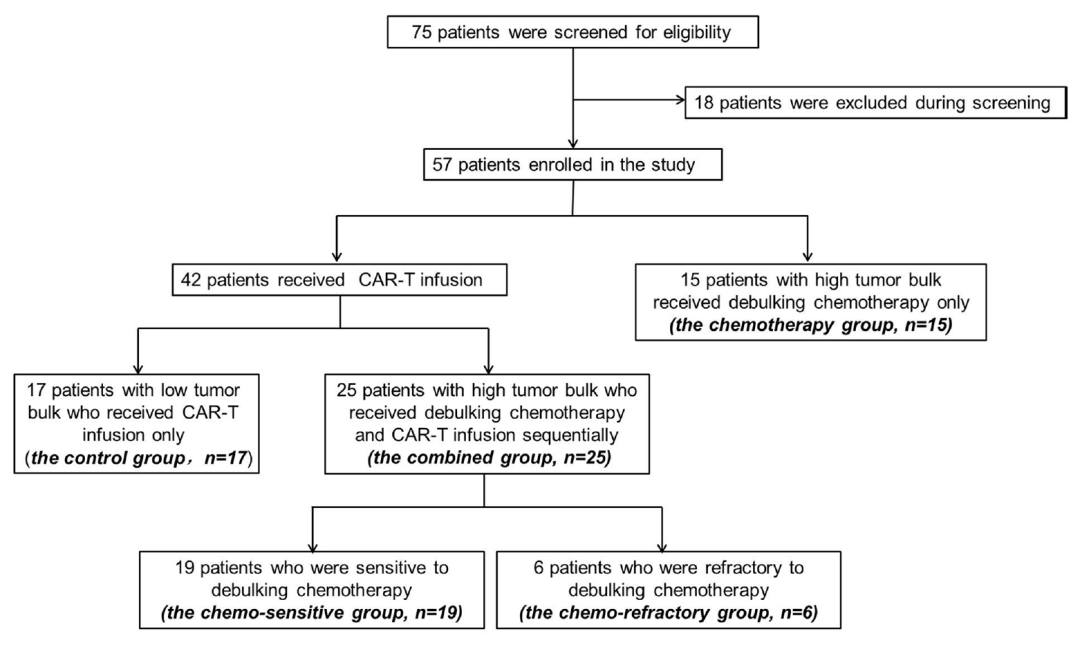
研究团队招募了57名难治性/复发性(R/R)弥漫性大 B 细胞淋巴瘤(DLBCL)患者参与这项临床试验,其中15名高肿瘤负荷患者仅接受减瘤化疗。其余42名患者接受CAR-T细胞治疗(有17名患者肿瘤负荷低,直接进行CAR-T治疗,他们作为对照组)。
25名肿瘤负荷高的患者患者依次接受减瘤化疗和淋巴细胞清除化疗。其中19人对化疗敏感,6人对化疗耐药。然后接受人源化抗CD19-CAR-T细胞疗法治疗。
所有患者均在抗CD19-CAR-T细胞输注后2个月内接受评估。化疗敏感组的19人中有18人客观缓解(客观缓解率为95.0%),13人完全缓解(完全缓解率为68.4%)。化疗耐药组的6人中有3人客观缓解(客观缓解率为50.0%),其中3人部分缓解,3人疾病进展。
作为对照组的直接进行CAR-T细胞治疗的17名肿瘤负荷低的患者的客观缓解率为88%。完全缓解率为59%。

在接受CAR-T疗法的各组中,出现细胞因子释放综合征(CRS)的概率没有明显差异,没有患者出现神经系统毒性,且没有患者死于细胞因子释放综合征和神经系统毒性。
在接受CAR-T治疗的19名对化疗敏感的患者的1年无进展生存率和总生存率分别为52.6%和57.9%,这高于接受CAR-T治疗的6名对化疗耐药的患者,而且同样高于15名仅接受化疗减瘤的高肿瘤负荷患者。这也表明了,对于高肿瘤负荷的难治性/复发性(R/R)弥漫性大 B 细胞淋巴瘤(DLBCL)患者,单独的化疗减瘤并不能改善预后。

总的来说,这项临床试验表明,有效的化疗减瘤改善了高肿瘤负荷的患者的客观缓解率和总生存率,使其与低肿瘤负荷患者的结果相当。这也为高肿瘤负荷的难治性/复发性(R/R)弥漫性大 B 细胞淋巴瘤(DLBCL)患者的治疗提供了一种新的治疗方案——强化化疗减瘤和CAR-T细胞疗法联合治疗。
原始出处:
Cuicui Lyu, et al. Intensive Debulking Chemotherapy Improves the Short-Term and Long-Term Efficacy of Anti-CD19-CAR-T in Refractory/Relapsed DLBCL With High Tumor Bulk. Frontiers in Oncology,2021.

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#ERS#
31
#Oncology#
41
#CAR-#
35
#肿瘤负荷#
49
学习
69
#Oncol#
34
#生存率#
28
学习学习
60
学校里面
66
学习学习
53