PLoS Med:血液维生素D水平低,MS患病风险增加
2015-08-27 MedSci 译 MedSci原创
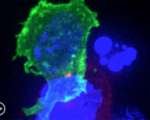
多发性硬化症委员会估计,美国有超过400000人患有多发性硬化症(MS)。MS是—种特定性地针对中枢神经系统白质,导致其脱髓鞘的自身免疫病。该病很难预测且进展速度和发病机理尚不清楚。它会对世界各地患病的年轻人造成永久性和难恢复的中枢神经系统损伤。既往研究表明,该病的发生和进展程度与遗传和环境等因素有关。来自加拿大麦克吉尔大学Brent Richards博士认为,血液中维生素D水平降低是促使该病发生
多发性硬化症委员会估计,美国有超过400000人患有多发性硬化症(MS)。MS是—种特定性地针对中枢神经系统白质,导致其脱髓鞘的自身免疫病。该病很难预测且进展速度和发病机理尚不清楚。它会对世界各地患病的年轻人造成永久性和难恢复的中枢神经系统损伤。
既往研究表明,该病的发生和进展程度与遗传和环境等因素有关。来自加拿大麦克吉尔大学Brent Richards博士认为,血液中维生素D水平降低是促使该病发生的危险因素之一。他说:“其他探究疾病模式的研究表明,机体血液中维生素D含量低会增加机体患MS的风险,但是不能证明维生素D含量低就一定会导致机体患MS。”
既往研究表明,因为高纬度地区日光照射不足,所以在那里居住的民众MS患病率更高。
麦克吉尔大学的研究人员也从遗传学的角度,着重研究血液维生素D含量低是否会造成民众MS易感性。他们对2347名多发性硬化症国际遗传学联合研究(MS遗传学研究的最大规模,包括14498名MS患者和24091名健康民众作为对照)的成员进行了评估,通过检测他们体内的25羟-维生素D含量作为他们的维生素D水平。
研究结果表明,在参与者中,所有欧洲血统的参与者维生素D水平低都会导致MS患病风险增加。但是目前还没有可以治愈疾病的药物,许多药物仅能用于治疗疾病所致的临床表现和伴随而来的其他重大健康风险。
Richards和他的同事认为,正在进行的随机对照研究主要用于评估维生素D补充治疗对MS治疗的效果和预防作用。但是仍需进行后续的研究,以避免MS的进展和对机体造成的更进一步的伤害。
原始出处:
Brent Richards et al.Vitamin D and risk of multiple sclerosis: A mendelian randomization study.PLOS Medicine.August 25 2015.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












不错,多学习!
80
学习了,很好
132
学习了,很好
151
学习了,很好
127
学习了,很好
128
学习了,很好
80
非常不错的基础文章。
97
M站的文章真心不错,基础、理论、临床都有!
36
#患病风险#
26
#Med#
22