CDS2018:糖尿病肾脏病诊治的新靶点——肾小管上皮细胞
2018-12-02 国际糖尿病编辑部 国际糖尿病
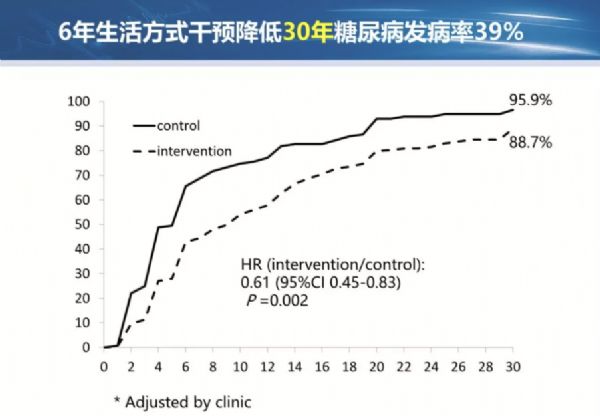
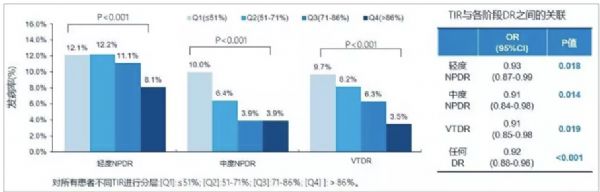
糖尿病所致的肾损害并不仅仅局限于肾小球,肾小管上皮细胞在糖尿病肾脏病(DKD)的早期和进展期均发挥了关键作用。2018年11月30日,在中华医学会糖尿病学分会第二十二次全国学术会议(CDS2018)上,南方医科大学南方医院薛耀明教授从DKD防治的严峻形势入手,介绍了肾小管上皮细胞在DKD发病中的重要性以及肾小管上皮细胞作为DKD治疗新靶点的最新研究进展。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#肾小管#
39
了解一下谢谢
86
#新靶点#
39
#糖尿病肾脏病#
37
#CDS#
36
#上皮细胞#
34
谢谢MedSci提供最新的资讯
55