JAHA:内脏静脉血栓形成与生存率的关联
2020-12-06 MedSci原创 MedSci原创
SVT比预期的更为常见。大多数患者患有癌症,门静脉是迄今为止最常见的受累静脉。与普通人群相比,SVT患者的生存期显著降低,尤其是在伴有癌症、肝硬化和既往有静脉血栓栓塞性疾病的患者中。
既往有关内脏静脉血栓形成(SVT)对患者生存率的研究十分有限。近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,这项研究通过链接到基于人群的数据,旨在评估一大型SVT患者队列的总体生存率。
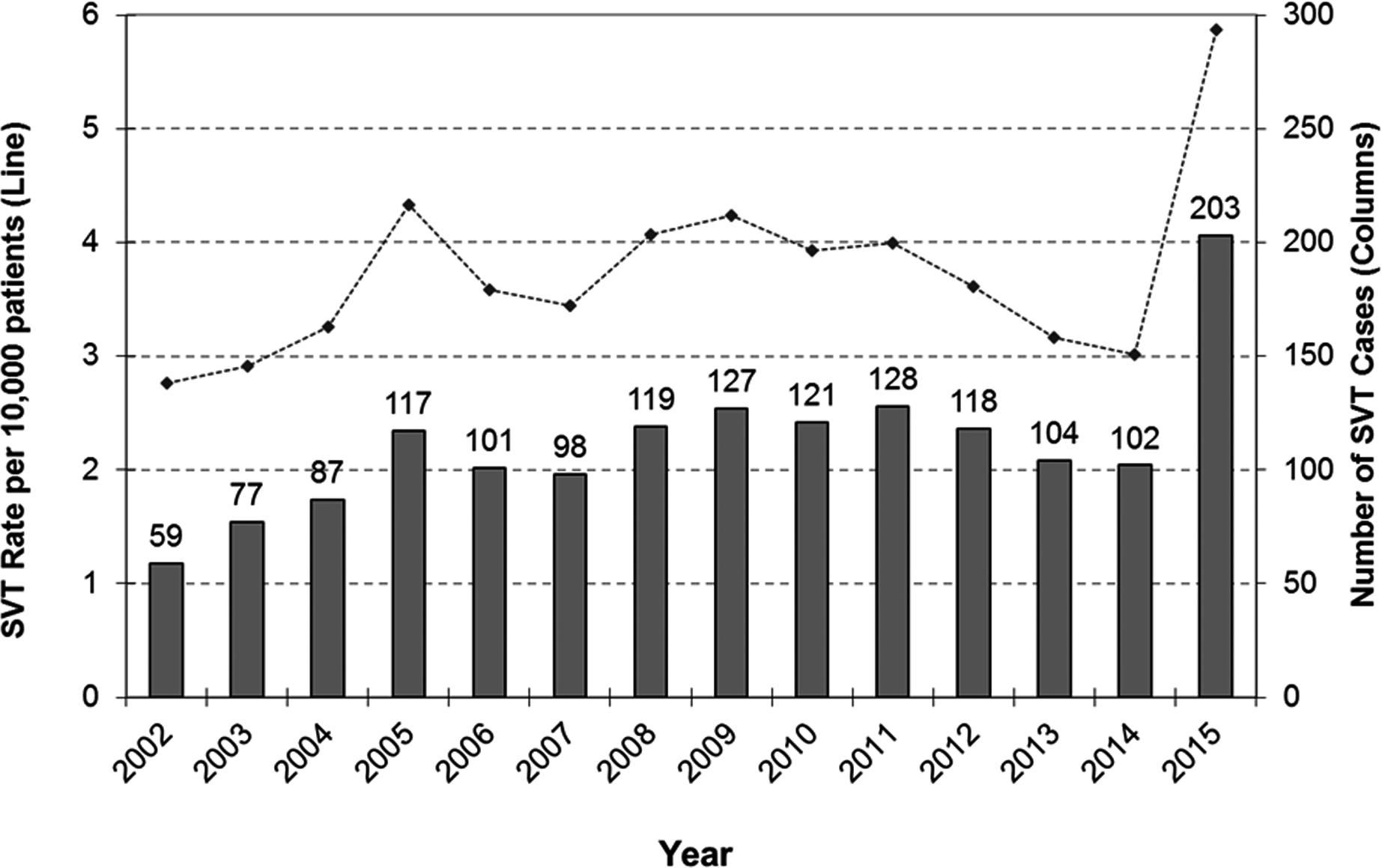
研究人员使用以前导出的文本搜索算法,筛选了渥太华医院历时14年的所有腹部超声检查和对比增强型计算机断层扫描检查的报告。筛查阳性报告由至少2位作者手动审核,以通过共识确定明确的SVT病例。不确定的检查图像由2位放射科医生独立审查。研究人员将1561名SVT成人(年发病率从2.8至5.9例/10000名患者)与基于人群的数据集联系起来,以评估伴随癌症的有无和生存状况。
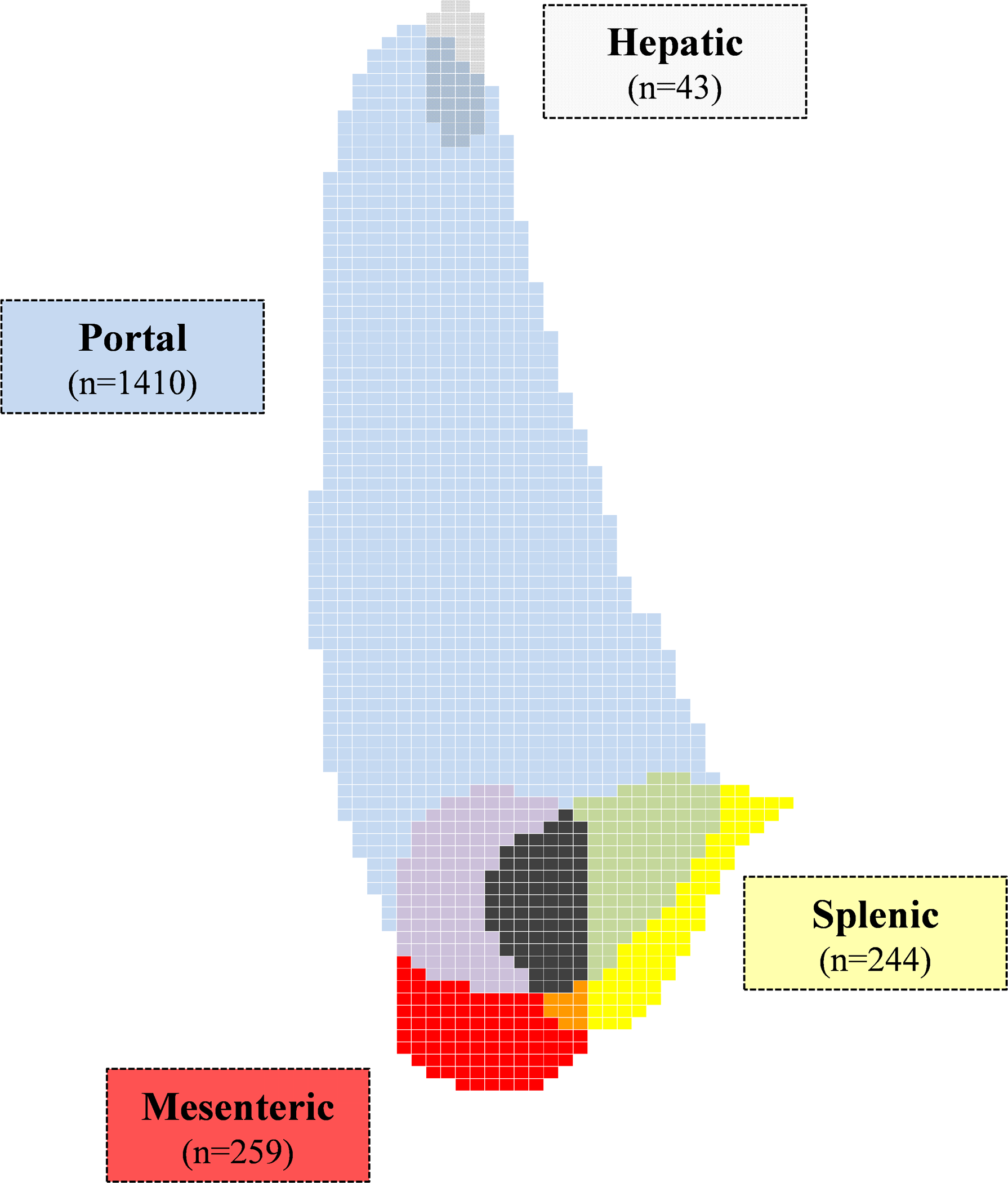
314例患者的血栓形成涉及多条静脉(占20.1%),最常见的是门静脉(n=1410,占90.3%)。
与同年龄性别匹配的人群相比,SVT患者的生存率显著降低,尤其是局部癌症(新发病例为12.0 [95%CI,9.8-14.6])、远处癌症(新发病例5.7 [4.5-7.3])、肝硬化(相对过高的风险8.2 [5.3-12.7])和既往有静脉血栓栓塞(相对过高风险3.8 [2.4–6.0])的患者中。在诊断的1个月内,有150名(23.9%)>65岁的患者接受了抗凝治疗。
由此可见,SVT比预期的更为常见。大多数患者患有癌症,门静脉是迄今为止最常见的受累静脉。与普通人群相比,SVT患者的生存期显著降低,尤其是在伴有癌症、肝硬化和既往有静脉血栓栓塞性疾病的患者中。大多数老年患者未接受抗凝治疗。
原始出处:
Philip S. Wells.et al.Association of Splanchnic Vein Thrombosis on Survival: 15‐Year Institutional Experience With 1561 Cases.J AM HEART ASSOC.2020.https://www.ahajournals.org/doi/full/10.1161/JAHA.120.016600
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#静脉#
34
#静脉血#
25
#生存率#
28
#AHA#
39
#静脉血栓形成#
40