European Radiology:超声引导下甲状腺和颈部活检术后出血并发症的预测
2022-06-04 shaosai MedSci原创
在淋巴瘤的诊断、唾液腺肿瘤的分化以及最初无法诊断或无法确定的甲状腺结节的确诊方面,US-CNB比US-FNA具有更大的优势
 超声(US)引导下的细针抽吸术(US-FNA)是诊断头颈部肿块的一种简便、安全、经济的技术,其诊断准确率为79-94.5%。研究证实,在淋巴瘤的诊断、唾液腺肿瘤的分化以及最初无法诊断或无法确定的甲状腺结节的确诊方面,US-CNB比US-FNA具有更大的优势。尽管最近的指南和文章表明,US- FNA和US-CNB的安全性和耐受性均较好,但这两种方法仍有可能伤及周围组织并导致出血。然而,大多数指南并没有为活检后的护理提供建议。
超声(US)引导下的细针抽吸术(US-FNA)是诊断头颈部肿块的一种简便、安全、经济的技术,其诊断准确率为79-94.5%。研究证实,在淋巴瘤的诊断、唾液腺肿瘤的分化以及最初无法诊断或无法确定的甲状腺结节的确诊方面,US-CNB比US-FNA具有更大的优势。尽管最近的指南和文章表明,US- FNA和US-CNB的安全性和耐受性均较好,但这两种方法仍有可能伤及周围组织并导致出血。然而,大多数指南并没有为活检后的护理提供建议。
近日,发表在European Radiology杂志的一项研究进一步明确了预测US引导下甲状腺和颈部活检术后出血性并发症的关键因素,为临床更好的管理及应用提供了参考依据。
本项回顾性研究分析了2020年4月至2020年11月期间接受US引导下活检的连续患者,比较了有和没有活检后出血患者的手术特征、US特征以及术前和术后患者的症状和体征。使用单变量和多变量回归分析,分析了临床和影像学变量与活检后出血之间的关联。
共纳入305名接受US引导下的甲状腺和颈部活检的患者(219名女性,86名男性;年龄范围,20-89岁)。17例(5.7%)活检后出血的病例是在活检和人工压迫30分钟后发现的。其中,10例在30分钟时出现出血,没有立即出血。在多变量分析中,活检后30分钟时视觉模拟量表(VAS)上的高触痛评分(几率[OR]5.05,P < .001)被确定为活检后出血的独立预测因素。在30分钟时有出血的患者中,在观察的30分钟内,触痛评分明显增加。
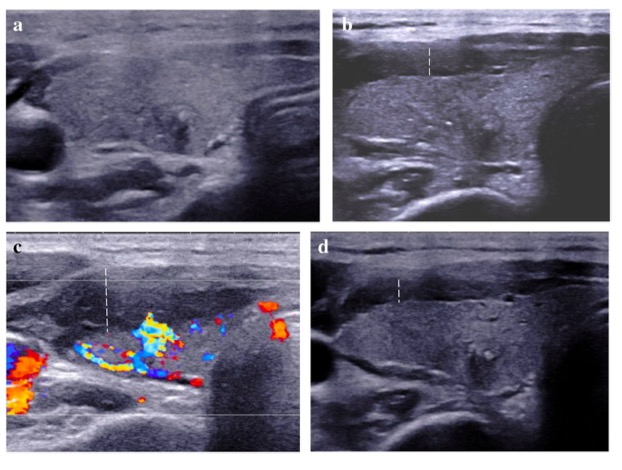
图 46岁女性,接受了甲状腺结节的核心针头活检。 a 在活检后立即进行超声检查(US),没有活检后出血的证据(疼痛评分3,触痛评分3)。b, c 手工按压后30分钟的US显示甲状腺周围有血肿(虚线,疼痛评分1,触痛评分4)。 d 1小时后的US显示甲状腺周围出血厚度减少(虚线)
本研究表明,30分钟的高触痛评分是US引导下甲状腺和颈部活检术后30分钟压迫出血的一个重要预测因素。因此,评估活检后30分钟的触痛评分可帮助操作者有效识别在US引导下甲状腺和颈部活检后需要进一步观察和处理的患者。
原文出处:
Ji Ye Lee,Ji-Hoon Kim,Hyun-Ah Chung,et al.Prediction of hemorrhagic complications after ultrasound-guided biopsy of the thyroid and neck.DOI:10.1007/s00330-021-08524-2
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#PE#
35
#并发#
41
#超声引#
34
#超声引导#
42
#活检#
53
#颈部#
38