Heart:降压药物对长期血压的影响
2022-06-18 MedSci原创 MedSci原创
这些研究结果表明,降压药物疗法对不同特征人群的降压效果平均长达4年。需要适当的治疗策略来维持实质性的长期降压效应。
药物治疗对长期血压(BP)降低的随机试验的证据十分有限。近日,心脏病领域权威杂志Heart上发表了一篇研究文章,研究人员旨在调查随着时间的推移和不同参与者特征的抗高血压药物对血压的影响。

研究人员使用混合模型对降血压治疗试验者协作组织中的52项大规模随机临床试验进行了个体患者水平的数据荟萃分析,以评估4年平均随访期间降压治疗对BP的影响。
该研究纳入了363684名参与者(42%为女性),基线平均年龄为65岁,平均收缩压/舒张压为152/87mmHg,其中19%为当前吸烟者,49%患有心血管疾病,28%患有糖尿病和69%的患者在基线时正在接受抗高血压治疗。药物在降低血压方面是有效的,在12个月后具有最大效果,并在以后几年逐渐减弱。
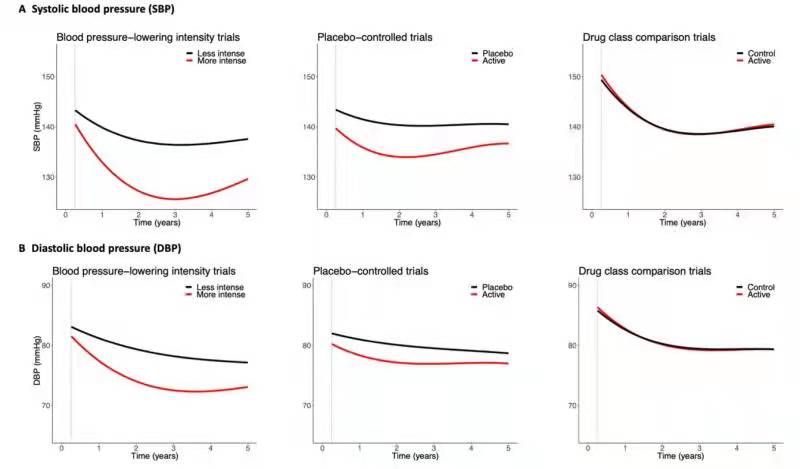
根据随机化后12个月以上采取的措施,更强和更弱的降压治疗之间的平均收缩压/舒张压差异(95%CI)为-11.1(-11.3至-10.8)/-5.6(-5.7至-5.4)mmHg;积极治疗和安慰剂之间为-5.1(-5.3至-5.0)/-2.3(-2.4至-2.2)mmHg;药物比较试验的积极组和对照组之间为-1.4(-1.5至-1.3)/-0.6(-0.7至-0.6)mmHg。在不同的基线血压值和年龄、性别、心血管疾病和糖尿病史以及既往抗高血压治疗情况下,研究人员观察到血压降低。
由此可见,这些研究结果表明,降压药物疗法对不同特征人群的降压效果平均长达4年。需要适当的治疗策略来维持实质性的长期降压效应。
原始出处:
Dexter Canoy.et al.Antihypertensive drug effects on long-term blood pressure: an individual-level data meta-analysis of randomised clinical trials.heart.2022.https://heart.bmj.com/content/early/2022/01/19/heartjnl-2021-320171
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#降压#
73
#ART#
70
#HEART#
73
学习#学习#
124