CHMP:Kisqali联合疗法扩展至所有HR + / HER2-局部晚期或转移性乳腺癌的女性
2018-11-19 MedSci MedSci原创
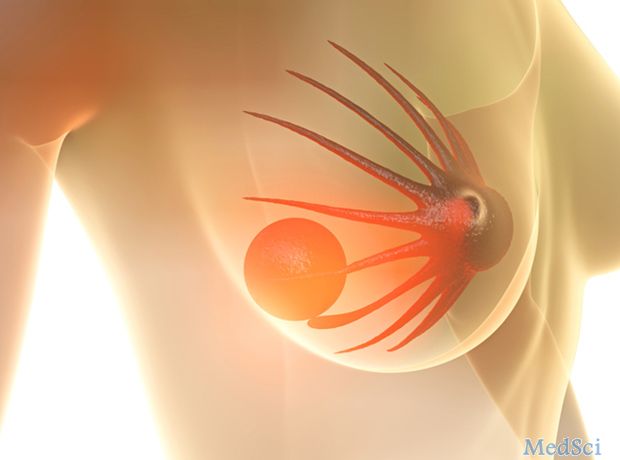
诺华公司近日宣布,欧洲药品管理局(EMA)的人用医药产品委员会(CHMP)采纳了积极的意见,建议扩大对Kisqali®(ribociclib)的适应症,这是一种CDK4 / 6抑制剂。CHMP推荐Kisqali与氟维司群联合用于治疗激素受体阳性 / 人类表皮生长因子受体-2阴性(HR + / HER2-)局部晚期或转移性乳腺癌患者。
诺华公司近日宣布,欧洲药品管理局(EMA)的人用医药产品委员会(CHMP)采纳了积极的意见,建议扩大对Kisqali®(ribociclib)的适应症,这是一种CDK4 / 6抑制剂。CHMP推荐Kisqali与氟维司群联合用于治疗激素受体阳性 / 人类表皮生长因子受体-2阴性(HR + / HER2-)局部晚期或转移性乳腺癌患者。积极意见还建议批准Kisqali联合促黄体激素释放激素激动剂(LHRH)用于围绝经期前和围绝经期的女性。
诺华公司肿瘤学公司首席执行官Liz Barrett说:“CHMP意见使我们更接近于在欧洲为更多HR + / HER2-晚期乳腺癌患者提供治疗选择”。CHMP的这一积极意见是基于第三阶段MONALEESA-7和MONALEESA-3试验的数据。MONALEESA III期试验招募了2000多名女性,这使得Kisqali成为迄今为止具有最广泛的一线临床试验证据的CDK4 / 6抑制剂。这些试验表明,与单独使用内分泌治疗相比,基于Kisqali的治疗方案可显著延长患者无进展生存期(PFS)。
原始出处:
http://www.firstwordpharma.com/node/1604998#axzz5XAXlsKfr
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Kisqali#
36
#联合疗法#
33
#HER2-#
31
#局部晚期#
36
#CHMP#
41
#转移性#
26
#局部#
21
学习了
51