颈静脉球瘤致寰枕关节失稳1例
2019-12-19 闻君侠 刘亦杨 王健 临床骨科杂志
患者,女,62岁,因发现左侧枕颈部肿块30年,声音嘶哑1个月于2018年2月20日入院。30年来肿块缓慢增大,无明显疼痛及其他不适。入我院前1个月因声音嘶哑于外院就诊,考虑甲状腺癌,行手术治疗,术后病理诊断为甲状腺乳头癌。术后1个月伴左耳听力下降,偶有喝水呛咳,无明显吞咽困难,体重无明显变化。体格检查:生命体征平稳,一般情况良好,胸腹未见明显异常。左侧枕颈部后外侧有一约5cm包块,边界欠清,质韧
临床资料
患者,女,62岁,因发现左侧枕颈部肿块30年,声音嘶哑1个月于2018年2月20日入院。30年来肿块缓慢增大,无明显疼痛及其他不适。入我院前1个月因声音嘶哑于外院就诊,考虑甲状腺癌,行手术治疗,术后病理诊断为甲状腺乳头癌。术后1个月伴左耳听力下降,偶有喝水呛咳,无明显吞咽困难,体重无明显变化。体格检查:生命体征平稳,一般情况良好,胸腹未见明显异常。左侧枕颈部后外侧有一约5cm包块,边界欠清,质韧,推之不移,无明显压痛,无明显波动感。颈椎屈伸活动轻度受限。鼻唇沟对称,伸舌左偏,左耳听力减弱。四肢肌力、肌张力及反射均未见明显异常。B超显示:左侧甲状腺中上极实质性不均质占位;左侧甲状腺下极占位,考虑腺瘤;左侧颈静脉内栓子形成;双侧颈部可见淋巴结。PET-CT:甲状腺左上极占位,FDG代谢异常增高,考虑甲状腺癌;左侧枕骨及C1骨质破坏伴软组织肿块形成,FDG代谢异常增高,考虑转移瘤。
讨论
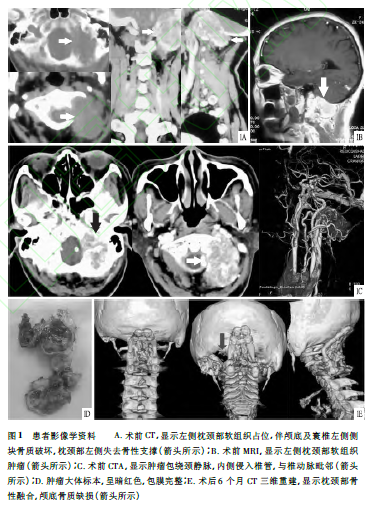
病理报告:左甲状腺符合甲状腺乳头状癌表现,颈后肿块可见恶性肿瘤细胞,考虑转移性癌。颈椎X线片显示:寰椎显影不满意,似可见骨质缺损。但CT及MRI检查均显示左侧枕颈部软组织肿瘤,肿块头端经颅底进入颅内,左侧颅底、寰椎侧块及前弓骨质破坏,枕颈部骨性失稳,见图1A、B。入院诊断:枕颈部转移癌?枕颈部转移性肿瘤伴寰枕关节失稳;甲状腺癌术后。入院后进一步行CTA检查,明确肿瘤大小、范围及其与邻近组织位置关系(见图1C)。联合神经外科制定手术方案,于全身麻醉下行左侧枕颈部肿瘤切除,自体髂骨混合同种异体骨植骨,AXON系统枕颈融合术。患者俯卧位,头部固定于Mayfield架,做左侧枕颈部耳后“门”字形切口,于胸锁乳突肌、斜方肌等颈后外侧肌深面显露肿瘤组织,见肿瘤呈暗红色,包膜完整,边界清楚;枕骨大孔左侧、寰椎左侧侧块及前弓左侧部分、枢椎左侧部分骨质缺损。结扎肿瘤周围营养血管,沿包膜分离,完整切除肿瘤,见肿瘤最头端经颅底进入颅内约2cm;尾端至C3下缘水平;前内侧头端至C1并突入椎管,紧贴椎动脉,尾侧紧靠C2,3椎体左侧;前外侧毗邻颈内动脉,并包绕颈内静脉;后外侧至乳突;枕颈部硬膜外可见明显肿瘤压迹。行枕颈部融合,融合范围颅底至C3,并取自体髂骨于枕颈部植骨。留置引流管。术中出血约1000ml。术后颈部制动,去枕平卧位休息。24h拔除引流管后,改头颈胸支具外固定,并下地负重活动。术中冰冻切片:无结构的上皮样组织。术后病理组织学诊断:未见恶性肿瘤细胞,上皮组织来源,副神经节瘤(颈静脉球瘤)首先考虑(见图1D)。予以修正诊断:颈静脉球瘤伴寰枕关节失稳;甲状腺癌术后。术后未针对肿瘤再行放化疗,佩戴头颈胸支具。术后3个月复查,部分骨性融合。术后6个月复查,枕颈部骨性融合(见图1E)。术后1年复查,枕颈部骨性融合,稳定性良好,未见肿瘤复发,但颈部屈伸及旋转活动受限。
原始出处:
闻君侠,刘亦杨,王健,金心,程有根,徐卫星.颈静脉球瘤致寰枕关节失稳1例[J/OL].临床骨科杂志,2019(06):763-764[2019-12-19].http://kns.cnki.net/kcms/detail/34.1166.R.20191212.0939.096.html.
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#静脉#
28
#寰枕关节#
30
好好好好好好
67
学习了很有用不错
65