Neuro Oncol.:脑膜瘤放疗后增强造影体积的增加反映了肿瘤的进展,而不是假进展
2021-06-23 MedSci原创 MedSci原创
脑膜瘤患者中出现假性进展的病例数量有限。该研究表明,在放疗治疗的脑膜瘤中,假进展可能很少见。
假性进展是一种治疗诱导的、对比增强肿瘤体积的短暂增加,与停止积极治疗或实施不必要的新治疗的风险相关。放射性脑膜瘤假进展的频率尚不清楚。
Neuro-Oncology杂志刊发论文,对2000年1月至2018年9月在一家三级转诊中心接受组织学证实的颅内脑膜瘤放射治疗的患者进行了纵向肿瘤体积分析。

使用Brainlab Elements V2.6软件(Brainlab, Munich, Germany)对磁共振成像的增强病变进行体积分析。影像学上,假性进展被先验定义为可测量目标病变增加10%的探索性截断量,或在辐射范围内出现新的造影增强病变(不需要新的最小增强体积),无进一步治疗的情况下,随后在1年内下降10%。进展根据神经肿瘤反应评估(RANO)标准确定。
在1235例1590例连续诊断的颅内脑膜瘤中,有174例(11%)接受了放射治疗。8例放疗后随访不到3个月的脑膜瘤和1例接受近距离放射治疗的脑膜瘤被排除在分析之外。
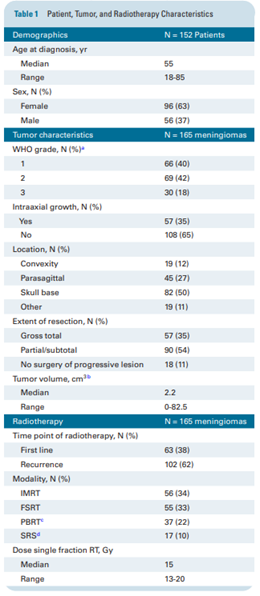
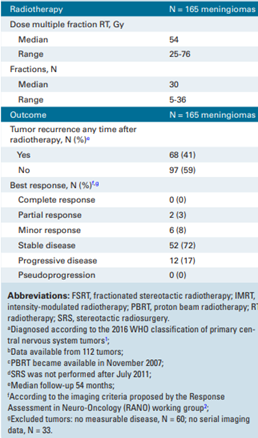
表1总结了152例患者中其余165例脑膜瘤的人口统计学和临床数据。在放疗后54个月的中位随访中,在中位30个月的时间间隔后,有68个放疗后脑膜瘤在放疗区域内进展,其中56个肿瘤在放疗前全切除,50个肿瘤被诊断为WHO 2级或3级。45例脑膜瘤,其中WHO 2级或3级肿瘤30例,放疗后再次切除,组织病理学一致证实肿瘤进展。选择颅底附近的脑膜瘤进行早期重复手术可能有先天的偏见。
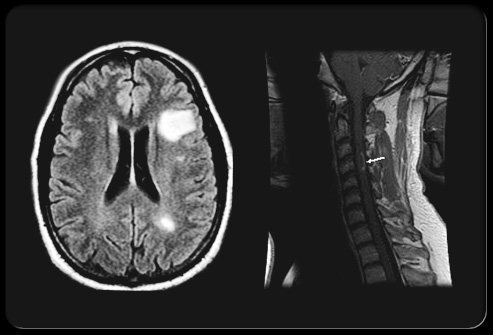
总的来说,在中位随访14个月(范围8-34)期间,在3-4个时间点对132个脑膜瘤进行了一系列肿瘤体积分析,未见新的造影增强病变自行消退。在开始放射治疗时被归类为可测量病变的72例脑膜瘤中,造影增强体积没有超过10%的瞬间增加。没有假进展的95%置信区间为0%-2.8%。在165个脑膜瘤群体中多学科肿瘤委员会怀疑1例WHO 1级脑膜瘤患者出现放射性坏死,原因是在立体定向放射治疗10次30 Gy再照射7个月后出现新的实质造影剂增强病变。立体定向放射治疗后4年进行再照射,54 Gy, 30次,贝伐单抗对疑似放射坏死有反应。
脑膜瘤患者中出现假性进展的病例数量有限。该研究表明,在放疗治疗的脑膜瘤中,假进展可能很少见。相比之下,20%-40%的前庭神经鞘瘤患者在立体定向放射手术后出现过短暂的体积扩大。该研究的主要局限性是被认为最有为假性进展的样本量小,WHO 1级脑膜瘤患者接受立体定向放射手术治疗(n = 7)并有足够的影像学随访(该亚组中位数为18个月)。在该研究中,大多数进展发生在WHO 2级或3级脑膜瘤中。然而,该研究分析表明,在大多数脑膜瘤患者中,由于放射治疗后怀疑出现假性进展而延迟再干预可能是不够的。
原文出处
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Oncol#
33
值得学习
53
#脑膜瘤#
48
#造影#
40
谢谢梅斯分享这么多精彩信息
59