Nat Commun:病毒也能治脑瘤
2019-05-30 晋楠 中国科学报
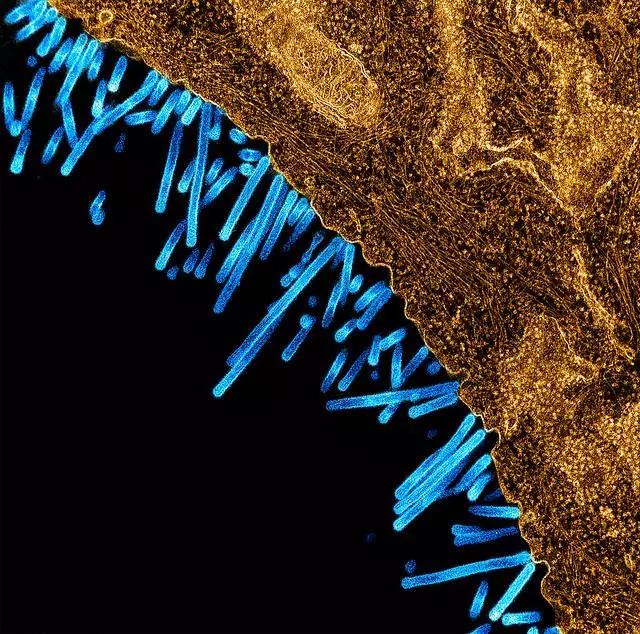
《自然—通讯》5月28日发表的一项研究称,一种溶瘤病毒(靶向癌细胞的病毒)有效延长了两种不同类型儿童脑肿瘤模型小鼠的存活时间。这些发现促使研究人员利用该病毒展开一项长期临床试验。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Nat#
27
#COMMUN#
20
#脑瘤#
36
好
73
不错
89