Lancet Respir Med:吸入性Treprostinil可明显改善间质性肺疾病和相关肺动脉高压患者的肺活量
2021-07-05 MedSci原创 MedSci原创
吸入性Treprostinil可明显改善间质性肺疾病和相关肺动脉高压患者的肺活量
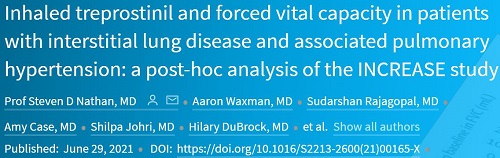
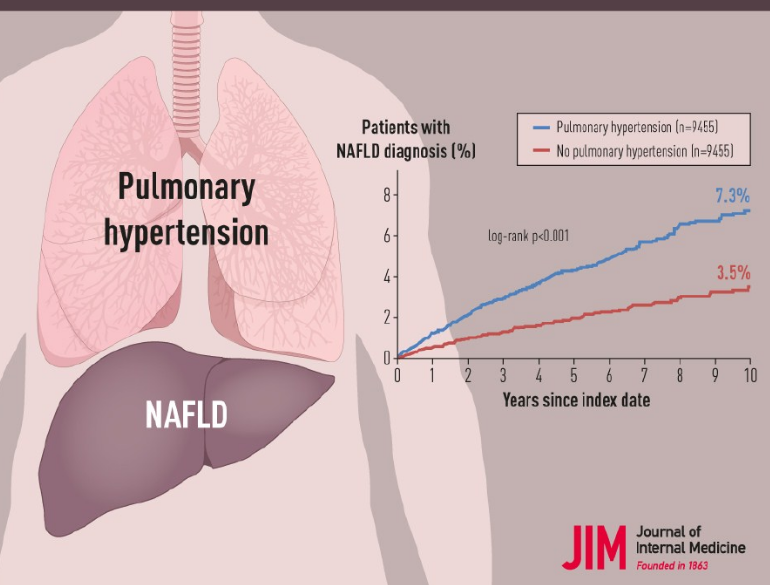
INCREASE试验是一项随机、安慰剂为对照的3期试验,旨在评估间质性肺病 (ILD) 和相关肺动脉高压患者应用吸入性Treprostinil的疗效和安全性。试验结果显示,与安慰剂相比,第16周时,Treprostinil较基线明显改善了患者的运动能力(6分钟步行试验);而且用力肺活量 (FVC) 也获得了一定改善。
本文报告了事后分析结果,此次分析旨在进一步表征吸入性Treprostinil对整个研究人群和各种亚组患者的FVC的影响。
在该分析中,研究人员评估了整个研究人群和由疾病原因或基线临床参数定义的各个亚组的FVC变化。受试患者为年满18岁的在6个月内经胸部CT检查显示弥漫性实质性肺疾病确诊的ILD患者。
总人群两组患者第8周和第16周时的FVC变化
2017年2月3日-2019年8月30日,INCREASE试验招募了326位患者。吸入性Treprostinil与FVC的经安慰剂校正的最小二乘平均改善相关,第8周和第16周时分别改善了28.5 mL(SE 30.1; 95%CI -30.8~87.7; p=0.35)和44.4 mL(35.4; -25.2~114.0; p=0.21);吸入性Treprostinil还与预测FVC改善的百分比相关(第8周和第16周时分别改善了1.8%[p=0.014]和1.8%[p=0.028])。
特发性间质性肺炎患者第8周和第16周时的FVC变化
特发性间质性肺炎患者的亚组分析显示,吸入性Treprostinil组和安慰剂组第8周和第16周时的FVC差分别为46.5 mL(SE 39.9;95%CI -32.5~125.5;p=0.25)和108.2 mL(46.9;15.3~201.1;p=0.023) 。对特发性肺纤维化患者的亚组分析显示,吸入性Treprostinil组和安慰剂组第8周和第16周时的FVC差分别为84.5 mL(52.7;-20.4~189.5;p=0.11)和168.5 mL(64.5;40.1~297·0;p=0.011)。
最常见的不良事件包括咳嗽、头痛、呼吸困难、头晕、恶心、疲劳和腹泻。
综上所述,ILD和ILD相关肺动脉高压患者采用吸入性Treprostinil治疗16周时,FVC可获得明显的改善。吸入性Treprostinil相比安慰剂的疗效差异在特发性间质性肺炎患者中最为明显,特别是特发性肺纤维化患者。吸入性Treprostinil可能是治疗特发性肺纤维化的一种很有前景的疗法,值得进一步深入研究。
原始出处:
Nathan Steven D,Waxman Aaron,Rajagopal Sudarshan et al. Inhaled treprostinil and forced vital capacity in patients with interstitial lung disease and associated pulmonary hypertension: a post-hoc analysis of the INCREASE study.[J] .Lancet Respir Med, 2021, https://doi.org/10.1016/S2213-2600(21)00165-X
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Lancet#
30
#肺活量#
33
#肺动脉高压患者#
29
#动脉高压#
24
#间质性#
32
#ROS#
31
#间质性肺疾病#
43
#PRO#
36
#Med#
34
学习了
64