Clin Cardiol:Evolucumab降低LDL-C(LAPLACE-2和RUTHERFORD-2试验)
2014-02-04 MedSci MedSci原创
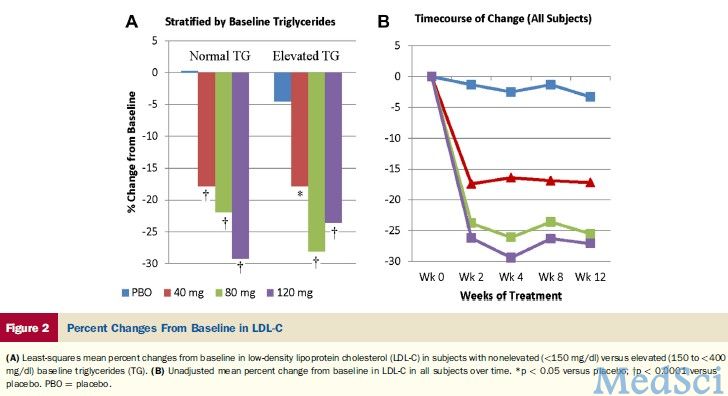
分别于1月28日和30日公布的LAPLACE-2和RUTHERFORD-2两项研究显示,Evolucumab可显著降低LDL-C水平。1. LAPLACE-2研究根据1月28日公布的LAPLACE-2研究结果,Evolucumab+他汀较单用他汀显著降低原发性高胆固醇血症和混合型血脂异常患者的LDL-C水平。Jennifer Robinson博士(爱荷华大学)将于2014年3月30日召开的美国
分别于1月28日和30日公布的LAPLACE-2和RUTHERFORD-2两项研究显示,Evolucumab可显著降低LDL-C水平。
1. LAPLACE-2研究
根据1月28日公布的LAPLACE-2研究结果,Evolucumab+他汀较单用他汀显著降低原发性高胆固醇血症和混合型血脂异常患者的LDL-C水平。Jennifer Robinson博士(爱荷华大学)将于2014年3月30日召开的美国心脏病学会科学会议(ACC2014)上公布该研究的完整结果。 Evolucumab(AMG-145)是一种作用于PCSK9的单克隆抗体。
LAPLACE-2研究纳入1896例高胆固醇血症和混合型血脂异常的患者。该研究是唯一的一项24个比较组的研究,包括Evolucumab 140mg,每2周一次/420mg,每月一次,安慰剂每2周一次/每月一次,或依折麦布,分别加用不同剂量他汀。
正如GAUSS-2、MENDEL-2和DESCARTES研究,LAPLACE-2研究达到了复合主要终点,包括第12周LDL-C较基线水平降低百分率和第10周、12周LDL-C平均降低百分率。
2. RUTHERFORD-2研究
1月30日RUTHERFORD-2研究公布结果,Evolucumab达到主要终点。该试验纳入了329例杂合子型家族性高胆固醇血症患者,随机分为4 组,包括皮下注射Evolucumab 140mg,每2周一次/420mg,每月一次,或安慰剂每2周一次/每月一次。该研究显示,不能耐受他汀治疗的患者使用Evolucumab可显著降低 LDL-C水平。
原始出处:
Robinson JG, Rogers WJ, Nedergaard BS, Fialkow J, Neutel JM, Ramstad D, Somaratne R, Legg JC, Nelson P, Scott R, Wasserman SM, Weiss R.Rationale and Design of LAPLACE-2: A Phase 3, Randomized, Double-Blind, Placebo- and Ezetimibe-Controlled Trial Evaluating the Efficacy and Safety of Evolocumab in Subjects With Hypercholesterolemia on Background Statin Therapy.Clin Cardiol. 2014 Jan 30. doi: 10.1002/clc.22252
Cho L, Rocco M, Colquhoun D, Sullivan D, Rosenson RS, Dent R, Xue A, Scott R, Wasserman SM, Stroes E.Design and Rationale of the GAUSS-2 Study Trial: A Double-Blind, Ezetimibe-Controlled Phase 3 Study of the Efficacy and Tolerability of Evolocumab (AMG 145) in Subjects With Hypercholesterolemia Who Are Intolerant of Statin Therapy.Clin Cardiol. 2014 Jan 29. doi: 10.1002/clc.22248.
Koren MJ, Giugliano RP, Raal FJ, Sullivan D, Bolognese M, Langslet G, Civeira F, Somaratne R, Nelson P, Liu T, Scott R, Wasserman SM, Sabatine MS; OSLER Investigators.Efficacy and Safety of Longer-Term Administration of Evolocumab (AMG 145) in Patients With Hypercholesterolemia: 52-Week Results From the Open-Label Study of Long-Term Evaluation Against LDL-C (OSLER) Randomized Trial.Circulation. 2014 Jan 14;129(2):234-43.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#mAb#
34
#ACE#
25
#LAP#
42
#Cardiol#
37
#LDL#
35
#APL#
33