Cancer Letters:德国科学家发现可有效抗癌的候选新药
2017-01-05 佚名 生物谷
本文亮点: BAY 1143269是一种具有强力作用和特异性的MNK1小分子抑制剂新药物 BAY 1143269能够强烈抑制MNK1底物eIF4E的磷酸化 参与肿瘤发生的MNK1下游靶点能够被BAY 1143269下调 在体内实验中,BAY 1143269单独治疗能够在肿瘤异种移植模型上表现出显著效果 BAY 1143269与化疗药物联合可以延缓体内肿瘤的再生长 最近,来自德国的科
本文亮点:
BAY 1143269是一种具有强力作用和特异性的MNK1小分子抑制剂新药物
BAY 1143269能够强烈抑制MNK1底物eIF4E的磷酸化
参与肿瘤发生的MNK1下游靶点能够被BAY 1143269下调
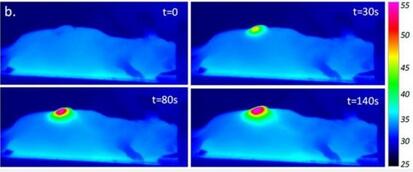
在体内实验中,BAY 1143269单独治疗能够在肿瘤异种移植模型上表现出显著效果
BAY 1143269与化疗药物联合可以延缓体内肿瘤的再生长

最近,来自德国的科学家们在国际学术期刊Cancer Letters上发表了一篇新文章,他们在这篇文章中介绍了一种新型抗肿瘤小分子药物能够通过抑制MNK1的激酶活性达到抗癌效果。
最近几年,mRNA翻译起始过程作为一种开发癌症治疗方法的新靶点得到了越来越多的关注。癌基因产物eIF4E是MNK1的一种主要底物,也是癌症相关PI3K和MAPK信号途径的交汇点。而MNK1也与细胞转化和肿瘤发生有密切关联,因此MNK1成为开发癌症治疗方法的一个很有前景的新靶点。
在这项研究中,研究人员通过高通量筛选和先导优化过程找到了一种新型MNK1小分子抑制剂——BAY1143269。在激酶实验中,BAY1143269表现出对MNK1的强力和特异性抑制。通过靶向MNK1的激酶活性,这种小分子药物还会强烈调节MNK1下游参与细胞周期,细胞凋亡,免疫应答和上皮间充质转化的因子,并且这种作用在体外和体内实验环境下都存在。除此之外,单独使用BAY1143269对癌细胞系和人源非小细胞肺癌异种移植模型表现出非常强大的作用效果,与标准化疗方法联合使用还可以阻止肿瘤的再生长。
这些结果表明,BAY1143269是一种强力并且特异性的MNK1小分子抑制剂,能够通过抑制MNK1的激酶活性影响参与肿瘤发生的其他因子。该研究为癌症治疗提供了新的候选药物。

原始出处:
Santag S, Siegel F, Wengner AM, Lange C, Bömer U, Eis K, Pühler F, Lienau P, Bergemann L, Michels M, von Nussbaum F, Mumberg D, Petersen K.BAY 1143269, a novel MNK1 inhibitor, targets oncogenic protein expression and showspotent anti-tumor activity.Cancer Lett. 2016 Dec 30. pii: S0304-3835(16)30799-6. doi: 10.1016/j.canlet.2016.12.029.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#ERS#
26
#科学家发现#
31
#TTE#
29
感谢分享一下!
62
#德国#
33