Eur Heart J:银屑病关节炎、银屑病和类风湿关节炎患者静脉血栓栓塞的风险如何?
2017-04-23 xing.T MedSci原创
由此可见,虽然全身炎症是VTE的危险因素,与对照者相比,发生VTE的风险在三种不同的炎症性疾病:类风湿关节炎、PsA和牛皮癣的患者中是不同的。
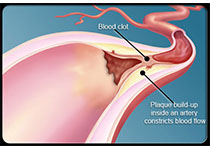
近日,心血管领域权威杂志Eur Heart J上发表了一篇研究文章,该研究旨在确定银屑病关节炎(PsA)、银屑病和类风湿关节炎(RA)患者相比于对照人群的静脉血栓栓塞(VTE)风险,VTE定义为深静脉血栓形成(DVT)和肺栓塞(PE)的复合终点。
研究人员采用英国的初级保健病历数据库中1994年至2014年期间PsA、RA或银屑病患者的数据进行了一项队列研究。通过Cox比例风险模型来计算DVT、PE和VTE的相对危险性。预先假设与疾病修饰抗风湿药物(DMARD)的相互作用是先验的并且显著的。PsA患者(n=12084)、RA(n=51762)、银屑病(n=194288)和对照者(n=1225571)一般情况均相匹配,并且确定了开始的日期。
研究人员发现RA患者(有或无DMARD处方)和轻度银屑病患者VTE风险显著增加(风险比分别为1.35、1.29和1.07),当对传统的危险因素进行调整后。给予DMARD处方的重度牛皮癣和PsA患者VTE风险有所升高,但不显著。DVT结果是相似的。年龄和性别调整后,给予DMARD处方的RA、重症银屑病和PsA患者发生PE的风险升高。
由此可见,虽然全身炎症是VTE的危险因素,与对照者相比,发生VTE的风险在三种不同的炎症性疾病:类风湿关节炎、PsA和牛皮癣的患者中是不同的。
原始出处:
Alexis Ogdie, et al. Risk of venous thromboembolism in patients with psoriatic arthritis, psoriasis and rheumatoid arthritis: a general population-based cohort study. Eur Heart J. https://doi.org/10.1093/eurheartj/ehx145
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#静脉#
30
#静脉血#
33
#类风湿关节炎患者#
32
学习了,谢谢
77
学习内容
65
学习了谢谢了。
58
#关节炎#
27
#类风湿#
25
#ART#
24
#HEART#
27