Aging and disease:华中科技大学协和医院团队揭开COVID-19肾损伤临床特点及转归
2022-06-29 影像小生 MedSci原创
COVID-19并发AKI患者比非AKI患者有更高的总死亡率和更短的生存时间。AKI/CKD合并COVID-19感染患者预后较只合并AKI的COVID-19患者差。
SARS-CoV-2引起肺组织炎症,导致急性呼吸窘迫综合征(ARDS),类似于中东呼吸综合征冠状病毒(MERS-CoV)和SARS-CoV。肺是SARS-CoV-2的主要靶器官,肺炎是大多数COVID-19患者的初始临床症状。然而,这种病毒会导致多器官损伤。COVID-19可能涉及心脏、肝脏和肾脏等器官。中国、意大利和美国的早期临床研究报告显示,COVID-19患者的急性肾损伤(AKI)发生率在0.5% ~ 36.3%之间。前期研究发现,COVID-19患者肾损伤的病理表现包括弥漫性近端小管损伤伴刷状边界丢失、非等长空泡变性、明显坏死、明显的红细胞聚集阻塞毛细血管腔,无血小板或纤维样物质,以及冠状病毒颗粒聚集在小管上皮和足细胞。其他研究也观察到严重的急性肾小管坏死、SARS-CoV-2 NP抗原和含有病毒的空泡聚集在肾小管中。
Aging and disease刊发了华中科技大学同济医学院协和医院肾内科Jing Xiong等的研究文章,该研究收集并分析了2020年1月16日至4月16日在武汉协和医院西校区收治的1077例COVID-19患者的数据,调查了COVID-19患者中AKI和AKI在慢性肾脏疾病(AKI/CKD)的发病率,以描述这些患者的临床特征和结局,并确定与AKI发展相关的危险因素。
1077例COVID-19患者住院期间60例(5.6%)诊断为急性肾损伤(AKI),其中18例(30%)合并慢性肾脏疾病(AKI/CKD)。
COVID-19 AKI患者预后较差,重症监护室(ICU)入院率(28.3%)和病死率(65%)分别高于非AKI患者(3.4%和10.7%)。
在COVID-19患者中,AKI多发生在男性患者、老年人、病情较重患者及合并高血压、糖尿病、冠心病(CHD)、慢性阻塞性肺疾病(COPD)和CKD等合并症患者。
COVID-19 AKI患者较非AKI患者更易发生呼吸衰竭、消化道出血、急性肝损伤、急性心肌损伤、心力衰竭、急性呼吸窘迫综合征(ARDS)、脑血管意外和弥散性血管内凝血(DIC)。
与非AKI患者相比,COVID-19 AKI患者血小板计数、淋巴细胞计数、白蛋白水平和血清钙水平较低,但白细胞计数、中性粒细胞计数和血清钾水平较高。AKI患者的C反应蛋白(CRP)、白细胞介素-6 (IL-6)、降钙素原(PCT)等炎症指标明显高于非AKI患者。
与非AKI患者相比,COVID-19 AKI患者的凝血酶原时间(PT)更长,活化部分凝血酶活时间(APTT)更长,D-二聚体水平更高。
生存分析显示,COVID-19 AKI患者的生存率低于非AKI患者。此外,COVID-19 AKI/CKD患者的生存率低于只有AKI或CKD的患者。
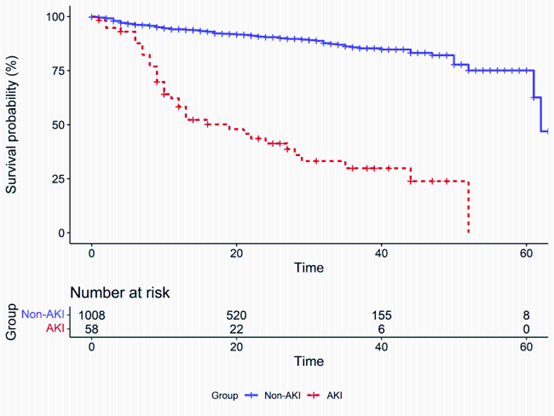
AKI和非AKI患者的生存曲线
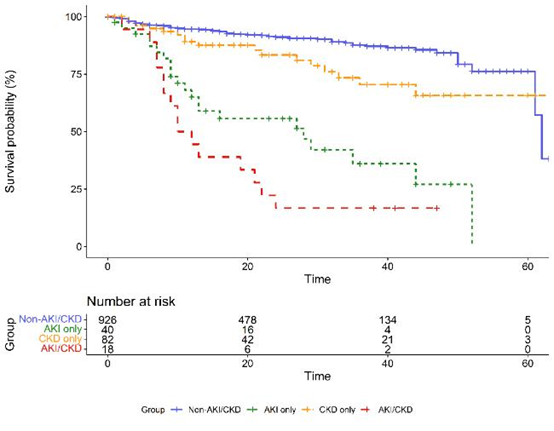
不同AKI和CKD患者的生存曲线
多因素logistic回归分析显示,呼吸衰竭、急性心肌损伤、住院期间肌酐和PCT水平升高等并发症是COVID-19患者AKI的预测因素。
总之,该研究发现COVID-19并发AKI患者比非AKI患者有更高的总死亡率和更短的生存时间。AKI/CKD合并COVID-19感染患者预后较只合并AKI的COVID-19患者差。还发现COVID-19患者的AKI与呼吸衰竭、急性心肌损伤肌酐和PCT水平密切相关。COVID-19急性肾损伤患者出院后的远期预后需要进一步研究。
原文出处
Zhifeng Xu , Yuanyuan Zhang , Chun Zhang , Fei Xiong , Jianduan Zhang , Jing Xiong. Clinical Features and Outcomes of COVID-19 Patients with Acute Kidney Injury and Acute Kidney Injury on Chronic Kidney Disease. Aging and disease. 2022, 13(3): 884-898 https://doi.org/10.14336/AD.2021.1125
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Dis#
34
#临床特点#
40
#协和#
47
#损伤#
43
#协和医院#
50